As far back as I can remember, I’ve wanted to help people with their health. I grew up watching my mom work as a medical doctor, and always admired her. In elementary school, I was introduced to the scientific method and thought: “This is it! This is what I’m going to do when I grow up!”
I enrolled in a four-year PharmD program (Doctor of Pharmacy) and became a pharmacist with the goal that one day, I would be able to discover new treatments for people who were suffering.
After I was diagnosed with Hashimoto’s, I decided to take my health into my own hands. I had been told that the only way to improve my health was to become dependent on thyroid medications, but I knew there had to be another way to feel my best and thrive. After months of research, I pinpointed lifestyle and dietary changes I could make to heal and reverse my Hashimoto’s.
After implementing these carefully researched lifestyle changes, I was able to see a tremendous improvement in my health.
Knowing there were others who also had thyroid conditions, and wanting to spread the message, I decided to summarize my research and improvements in my book, Hashimoto’s: The Root Cause, in 2013.
When I initially published the book, I was hopeful that one day a group of researchers would take the information I collected, and carry out a large-scale clinical trial to test the interventions.
Unfortunately, these types of clinical trials can be very expensive, and there isn’t a financial incentive for most companies to do this kind of research if they can’t collect a return on their investment.
Then in 2015, I realized that we, the thyroid community, have the power to conduct our own research! After all, I’ve found a tremendous amount of value from simply listening to people with Hashimoto’s.
I’ve learned so much from my clients and readers.
So, I developed a survey to assess the impact of various interventions, from dietary to lifestyle changes, on Hashimoto’s. 2232 people with Hashimoto’s took part in this survey and answered questions about factors that seemed to make their conditions better, and the factors that made their conditions worse.
In this article (which was originally published in 2015), we’ll dive into the results of the survey and discuss some important considerations for those with Hashimoto’s, including:
- How stress contributes to Hashimoto’s
- Nutrition as a key step to healing Hashimoto’s
- How supplements and lifestyle changes can accelerate healing
- Optimal ranges for thyroid hormone levels
- Why Low-Dose Naltrexone (LDN) can make a big difference for some individuals
1. Stress is a Huge Contributing Factor
The first takeaway that I want to share with you is that stress can be a major player in Hashimoto’s. Of those who took my survey, 69 percent reported a lot of stress in their life before they began to feel unwell.
Getting enough sleep, spending time with loved ones, being in nature, walking, getting a massage, reading, sitting on a beach, and being warm, were some of the activities that made most people with Hashimoto’s feel better.
On the other hand, having a lack of sleep, being stressed out, being around negative people, fighting with loved ones, having a lack of sunshine, and being in cold weather, made most people with Hashimoto’s feel worse.
When in a stressed state, our bodies can shift from a parasympathetic (resting) state, to a sympathetic (fight-or-flight) state. A part of our brain called the hypothalamus sets off a cascade of signals that eventually leads to the adrenal glands pumping out stress hormones. In the case of immediate stress, this response shuts off once the stressor is gone or has subsided.
However, when we’re chronically stressed, the adrenals are constantly pumping out stress hormones, and we’re constantly in a high-stress state. To meet the demand for cortisol, our bodies will produce additional hormones, such as DHEA, testosterone, and progesterone.
Over time, the negative feedback system that prevents our bodies from producing too much stress hormones, becomes desensitized and shuts off. When this happens, our bodies start focusing on the stressor and redirects our resources to meet the stress-induced demand for cortisol and adrenaline. As so many resources start going towards supporting these “survival” hormone pathways, they are taken away from other “less vital” functions — like growing beautiful hair, metabolizing nutrients into energy, making hormones, digesting, and generally repairing themselves.
The process described above can lead to a state known as adrenal fatigue. Stress can be a cause of adrenal fatigue that is often experienced with Hashimoto’s.
Please don’t underestimate the importance of stress reduction in your healing journey!
I want you to remember that stress is not just caused by external factors, but can also be self-induced due to our thought patterns like negative self-talk, rumination, and perfectionism.
Causes of stress can of course vary widely between individuals, but these are four of the most common causes that I see in those with Hashimoto’s:
- Sleep deprivation (sometimes caused by sleep apnea) can be a big trigger for stress. Many people may not be aware that they have a sleep disorder, so it’s important to get this checked out as a possible root cause.
- Anxiety and depression are characteristics or types of chronic emotional stress, and both are common in Hashimoto’s.
- Metabolic/glycemic dysregulation caused by blood sugar imbalances can greatly affect mood and contribute to stress.
- Pain caused by chronic inflammation can be a key cause of stress — read my article on natural solutions for managing pain with Hashimoto’s for more information.
It’s important to get to the root of your stress to really heal, and the causes can be complex. But even if you don’t know the root cause(s) quite yet, there are many simple steps you can take to reduce stress in your life.
I recommend taking a nice vacation or “staycation” where you take a few days to focus on self-care, and practice relaxation activities such as meditation and sauna therapy.
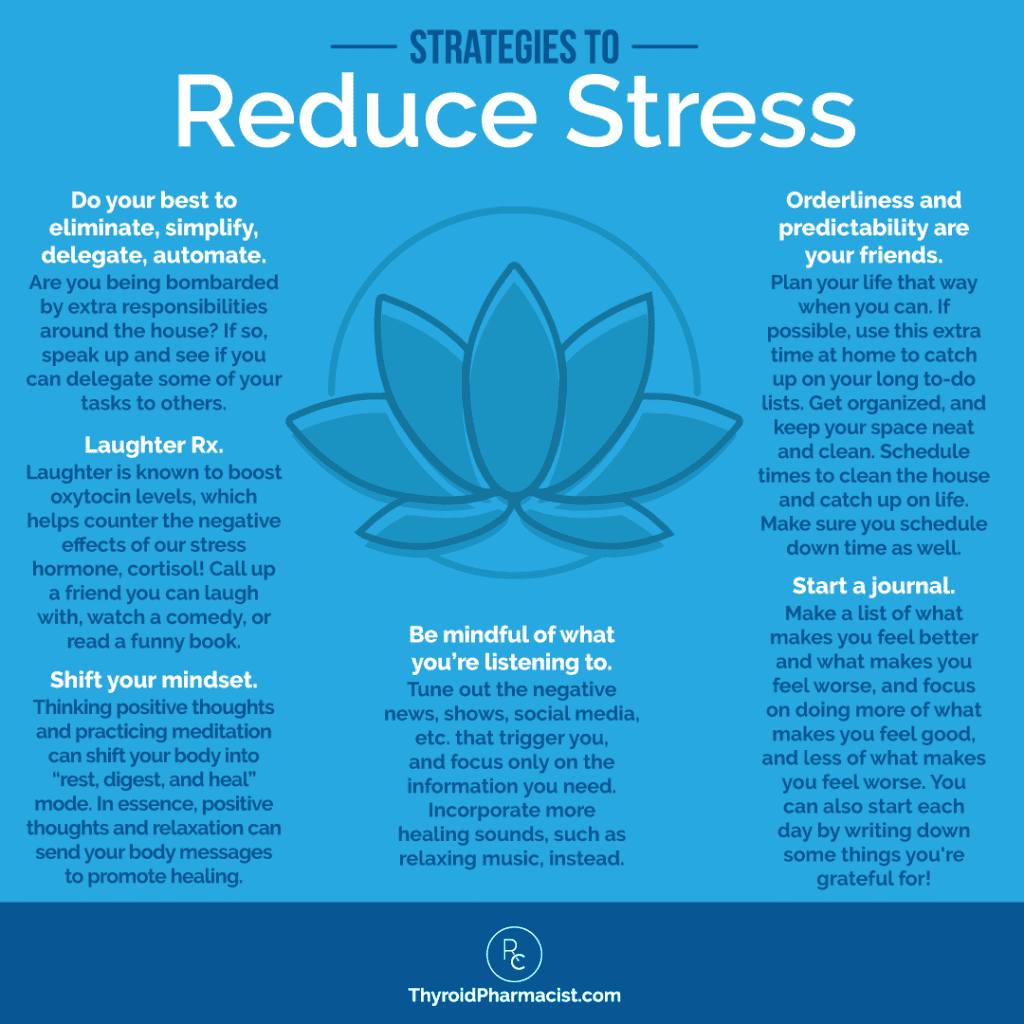
Other methods to reduce stress include:
- Do your best to eliminate, simplify, delegate, automate so you can reduce your to-do lists and commit to a reasonable number of responsibilities.
- Shift your mindset to practice positive thoughts and affirmations.
- Be mindful of what you’re listening to.
- Schedule, plan and get organized… because orderliness and predictability are your friends.
- Laugh — laughter is the best medicine, besides food. #LaughterRx
- Start a journal.
- Consider taking adaptogens to combat stress.
If you’re interested in learning about these methods and want a more in-depth approach to reducing stress, check out my article on stress and adrenal fatigue.
2. Nutrient Deficiencies Can Contribute to Many Symptoms
Nutrition is a key piece in healing Hashimoto’s. When nutrition isn’t optimal, nutrient deficiencies can arise, affecting thyroid function and contributing to symptoms of Hashimoto’s. My survey results reflected three major deficiencies that are generally common in Hashimoto’s: 68 percent, 33 percent, and 28 percent were found to have low levels of vitamin D, low levels of B12, and low levels of ferritin, respectively. These are all vital for thyroid function.
Vitamin D supports the immune system by enhancing the pathogen-fighting effects of white blood cells, which are important parts of immune defense. Vitamin D also reduces the risk of respiratory infections.
Numerous studies have connected low vitamin D levels to various autoimmune conditions. In particular, research has shown that lower levels of vitamin D are associated with higher thyroid antibodies (TPO and TG antibodies). Healthy levels of vitamin D, meanwhile, can reduce antibody levels. (Read my article on vitamin D for more information.)
Low ferritin levels, which may indicate iron-deficiency anemia, can contribute to hair loss, among other symptoms. A 2005 Iranian study published in the Asia Pacific Journal of Clinical Nutrition examined the effect of low iron on young women, by collecting urine and serum samples of iron-deficient adolescent girls. The results concluded that there was a significant correlation between the T4, TSH, and ferritin levels studied in the subjects. Iron is responsible for creating T4 and converting T4 to the more active T3 thyroid hormone, and the results of this study suggested that iron deficiency may affect thyroid hormone status in adolescent girls. (Learn more about low levels of ferritin and hair loss here.)
Lastly, B12 deficiency can also affect thyroid function, as it is important for energy, protein synthesis, cell reproduction, and normal growth. Low levels or levels closer to the lower range of what’s considered normal, are associated with neurological symptoms such as difficulty balancing, memory lapses, depression, and fatigue… all of which are commonly seen with Hashimoto’s. (Learn more about low levels of B12 here.)
I cover the effects of these nutrient deficiencies more in-depth in the nutrient deficiencies chapter of my book Hashimoto’s: The Root Cause, which you can download for free by signing up here.
Do you have deficiencies in vitamin D, ferritin, B12, or other nutrients as well? The good news is that there is something you can do to combat these deficiencies. Taking supplements can help restore your nutrient levels and help improve the symptoms associated with Hashimoto’s.
Addressing nutrient deficiencies can reverse many symptoms associated with Hashimoto’s. Of note, it can help with fatigue, a common symptom experienced by many of the people who took my survey.
Here’s what the survey results showed:
See my article on the seven most common nutrient deficiencies in Hashimoto’s to discover other common nutrient deficiencies seen in Hashimoto’s, the supplements that I recommend to optimize levels, and how to supplement appropriately.
3. Gluten Sensitivity with Hashimoto’s is a Big Deal
If you’ve been following my research, you’ll know that gluten is one of the biggest triggers of symptoms seen in those with Hashimoto’s.
Gluten can have a significant impact on the thyroid because of a phenomenon called molecular mimicry, which works like this: gluten can leak into the bloodstream, as it can create permeability in the gut barrier. When it leaks into the bloodstream, the body does not recognize it, and labels the structure as a foreign invader and attacks it. However, because gluten, or more specifically the protein gliadin within gluten, mimics the structure of the thyroid, the body starts an attack on the thyroid as well.
Seventy-six percent of those who took my survey reported a gluten sensitivity (16 percent were not sure; the rest did not believe themselves to be sensitive).
Most people that reacted to gluten felt the reaction in their gut (symptoms of constipation, diarrhea, cramping, bloating, nausea, gas, acid reflux, burning or burping) and in the brain (with related symptoms such as headaches, dizziness, brain fog, anxiety, depression, fatigue, and insomnia).
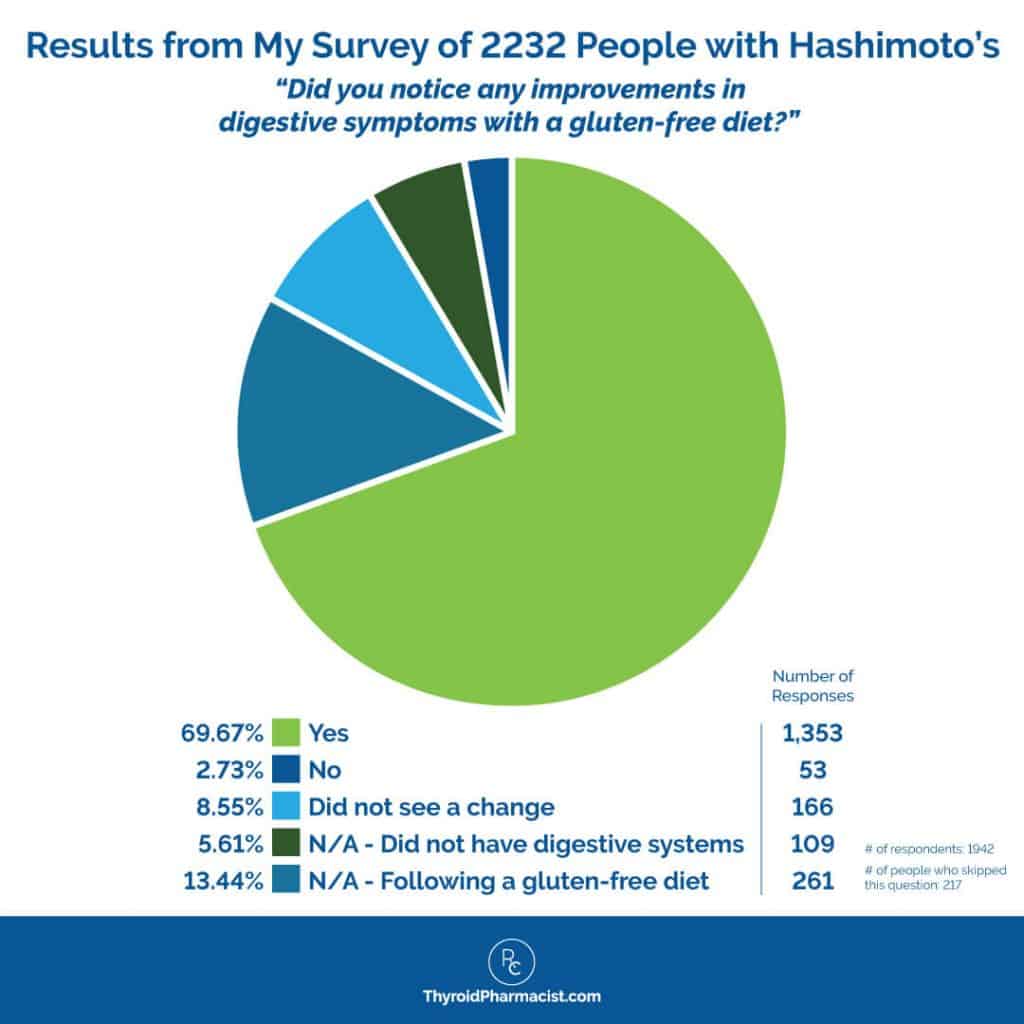
Overall, 88 percent of people who went gluten free felt better! And 86 percent of people who went gluten free reported an improvement in digestive symptoms. Notably, only 3.5 percent of survey respondents were diagnosed with celiac disease. This confirms what many of us in the world of functional medicine believe to be true: you do not have to have celiac disease to benefit from a gluten-free diet.
Thyroid antibodies were also reduced on a gluten-free diet, as 33 percent of respondents reported. Along with feeling better and seeing a reduction in antibodies, the biggest benefits seen in people with Hashimoto’s on the gluten-free diet were more energy (in 67 percent of people), a better mood (in 60 percent of people), and a healthier weight (in 52 percent of people).
Less than one percent of respondents reported feeling worse after going on a gluten-free diet, and 11 percent reported no noticeable changes.
I was not surprised to see these results.
One reader wrote:
“Gluten elimination was the first thing I did. I lost 8 pounds in 2 weeks without dieting. I added supplements, exercise, and cut out sugar. I’m still losing weight and cannot believe how good I feel!”
If you are still on the fence about changing to a gluten-free diet, I encourage you to try it! For more information, check out my article on gluten and Hashimoto’s.
When I first set out to feel better with Hashimoto’s, the research for the benefits of the gluten-free diet and Hashimoto’s was still emerging. I came across one study of the gluten-free diet helping people resolve their thyroid issues if they also had co-occurring celiac disease. I am glad that I tried the diet, that it helped me, and that I went on to share it with others!
Interestingly, Dr. Robert Krysiak and colleagues from the Department of Internal Medicine and Clinical Pharmacology at the Medical University of Silesia in Katowice, Poland, published an article about the benefits of the gluten-free diet in Hashimoto’s in 2019. ? I don’t know if this is a coincidence or not, but I was a keynote speaker at Poland’s first functional medicine and nutrition conference in 2016, and my book Hashimoto’s Protocol was a bestseller in Poland in 2017, so I would like to hope that maybe the scientists are listening to the patients that are reading my books!
Thirty-four women with autoimmune thyroiditis were split up into two groups, where one group followed a gluten-free diet for six months, and the other followed a regular diet. After six months, the group without dietary treatment had thyroid hormone levels similar as at the start. But the gluten-free group showed significantly reduced levels of thyroid peroxidase (TPOAb) and thyroglobulin (TgAb) antibodies. Although this is a small study, the researchers concluded that the results are strong enough to suggest that a gluten-free diet could reduce thyroid autoimmunity.
4. Dietary Changes Can Impact Our Healing of Hashimoto’s
In addition to the gluten-free diet, there are other diets that can help with Hashimoto’s. When asked about which diets improved Hashimoto’s, the respondents revealed that the most helpful dietary interventions included a sugar-free diet, the Paleo diet, and a grain-free diet, as 81 percent of those who had tried these diets felt better.
Here are some other notable results from the survey:
- When I surveyed my readers with Hashimoto’s, 40 percent of people reported already being dairy free, while 57 percent reported that they suspected they were sensitive to dairy.
- 79 percent of those who tried the dairy-free diet felt better. (This comes as no surprise, as dairy can often be difficult to digest and contribute to gut symptoms seen in Hashimoto’s.)
- Improvements that were reported by going dairy free included improved mood (46 percent), energy (54 percent), weight (41 percent), skin (37 percent), and pain (39 percent).
- Less than two percent of people surveyed reported feeling worse by removing dairy, while 34 percent saw no noticeable difference.
- 80 percent of people felt better on a grain-free diet that eliminates both gluten-containing grains like wheat, barley, and rye, as well as gluten-free ones like rice, quinoa, and millet.
- Of the people that took my survey, symptoms that improved by eliminating grains included energy (65 percent), mood (59 percent), weight (54 percent), and pain (44 percent).
- Less than one percent of people reported feeling worse after eliminating grains, while 19 percent saw no difference.
- The Autoimmune Paleo (AIP) diet, which eliminates grains along with other common food triggers, helped 75 percent feel better. (Certain foods omitted on the AIP diet, such as tomatoes and potatoes, can be inflammatory and are also common food sensitivities. Eliminating these foods on the AIP diet can help people reduce their symptoms!)
- Corn, in particular, was noted as a large sensitivity, as was gluten. Other food triggers included dairy (79 percent), eggs (48 percent), sugar (87 percent), and soy (63 percent).
- Of those who took my survey, 71 percent noticed an improved mood, 79 percent experienced more energy, and 60 percent reported positive weight changes on a Paleo-style diet.
- A low glycemic index diet helped 76 percent feel better. (Carbohydrates high on the glycemic index can result in blood sugar spikes, and blood sugar issues are common in those with Hashimoto’s.)
- Specifically, people who went on a low glycemic index diet reported improved mood (61 percent), energy (71 percent), and weight (53 percent).
- Less than three percent of people surveyed felt worse on this type of diet, while 22 percent didn’t notice a difference in their symptoms.
- A sugar-free diet was also found to be helpful.
- Of the people that I surveyed, 87 percent reported feeling better when they ditched the sugar from their diet.
- 65 percent saw improvements in their mood, 67 percent experienced more energy, 52 percent reported positive weight changes, and 29 percent improved the condition of their skin.
- Less than two percent reported feeling worse after removing sugar from their diets, while 12 percent saw no noticeable improvement.
- Homemade bone broth (which contains an abundance of minerals and amino acids that can help heal the gut) helped 70 percent of those that tried it.
- 62 percent saw an increase in energy; 57 percent, an improvement in mood; and 32 percent, an improvement in skin.
- Green smoothies made of thyroid-friendly ingredients helped 69 percent.
- 82 percent said that the smoothies gave them more energy, 60 percent claimed improved mood, and 40 percent noticed benefits for weight.
- Fermented foods (such as sauerkraut and other fermented veggies) helped 57 percent.
- The benefits were seen in energy (64 percent), mood (49 percent), and pain reduction (27 percent).
Finding a healing diet that works best for your needs, and focusing on nourishing bone broth, fermented foods, and green smoothies, can result in tremendous improvements.
For more information on which diets work best for those with Hashimoto’s, and how to incorporate nourishing healing foods into your daily routine, please read my full article on the topic!
5. Supplements Can Help
When asked about supplements, a number of you agreed that they’ve helped improve your symptoms! Many of these supplements helped respondents to address nutrient deficiencies mentioned previously, such as low vitamin B12, low vitamin D, and low ferritin.
Specifically, survey results revealed that:
- Taking a B12 supplement helped 76 percent feel better. Supplementing with B12 can help boost levels of this vitamin, thereby improving energy, brain function, and mood.
- Symptoms that saw the most improvement included energy (88 percent) and mood (56 percent). Only two percent of people surveyed said they felt worse while taking a B12 supplement, and 22 percent said they didn’t notice any changes.
- Vitamin D3 supplements helped 74 percent feel better. Supplementing with vitamin D can especially help to improve mood and cognitive function during the winter months, as well as improve immune function.
- In my survey, 64 percent saw improvements in mood, 19 percent experienced pain reduction, and 35 percent saw a reduction in antibody titers on vitamin D.
- Ferritin/iron supplements helped 63 percent feel better. Supplementing with ferritin or iron supplements can improve hair loss and address anemia.
- Of those surveyed, 83 percent saw improvements in energy, 36 percent experienced improved mood, and 21 percent saw improvements in their hair.
In addition to these supplements, survey respondents also found the following to be particularly beneficial:
- Digestive enzymes helped 73 percent feel better. Enzymes help our bodies to better digest the food we eat and can reduce symptoms such as bloating and constipation.
- Omega-3 fatty acid supplements helped 65 percent feel better. Supplementing with omega-3 fatty acids can help reduce inflammation, boost skin health, and provide our bodies with the precursors to balance hormones.
- Improvements noticed by those who incorporated omega-3 fatty acids into their diet included mood (53 percent), energy (50 percent), skin (38 percent), and hair (26 percent).
- Selenium helped 63 percent feel better. Supplementing with selenium can reduce thyroid antibodies, reduce thyroid-related symptoms, and improve anxiety levels.
- Of those who saw improvement in their symptoms, 58 noticed more energy, 48 percent experienced better mood, 37 percent improved their labs, and 25 percent saw positive results in their body weight. Another 4 percent reported that selenium made them feel worse, while 34 percent saw no changes.
- Betaine with Pepsin helped 59 percent feel better. Supplementing with betaine and pepsin can improve digestion, as well as reduce bloating and acid reflux.
- Fifty-eight percent experienced improved energy, 40 percent noticed less pain, while 35 percent saw an improvement in their mood.
- Curcumin helped 56 percent feel better. Supplementing with bioavailable curcumin can help reduce inflammation that is experienced with Hashimoto’s.
- Of those surveyed, 65 percent noticed less pain, 35 percent saw increased energy, and 34 percent experienced improved mood.
- Zinc helped 52 percent feel better. Supplementing with zinc can help repair intestinal permeability, prevent oxidative stress, and optimize thyroid hormone levels.
- Fifty-eight percent of those surveyed experienced more energy, 49 percent saw improvements in mood, and 25 percent noticed better skin.
- It’s also great for boosting our immunity! In fact, one reader even reached out to comment: “Zinc supplements immediately eliminated a long-standing thrush infection that was not successfully treated by four doctors in 2 years.”
- L-glutamine helped 51 percent feel better. Supplementing with L-glutamine can help strengthen the gut lining, improve leaky gut, and boost gut function.
6. Banishing the Blues and Pain with Lifestyle Changes is Possible
In addition to dietary changes and supplements, lifestyle changes can also have a significant impact on our thyroid health.
If you’re feeling tired, blue and in pain, I recommend having a spa day! Be sure to look for one that has infrared saunas.
Sauna therapy, which promotes sweating and in turn, helps us eliminate toxins (which are often found in higher amounts in those with thyroid disease due to impaired liver function), is one such lifestyle change that helped an overall 57 percent of those who tried it to feel better. The biggest benefits were seen in mood, energy, skin, and reduced pain levels.
However, please note that sauna use may not be recommended in specific circumstances, or for those with certain medical conditions. You can learn more about infrared sauna contraindications in my article on saunas and Hashimoto’s.
Massage therapy is another spa treatment that was found to have helped improve mood for 80 percent of people, reduced pain for 62 percent, and improved energy levels for 45 percent of people. If this option isn’t available to you, you can take a hot Epsom salt bath at home, and ask your partner to give you a massage. ?
For more information on improving your mood, please see my article on the root causes of depression in Hashimoto’s.
7. There is a Sweet Spot for TSH Levels
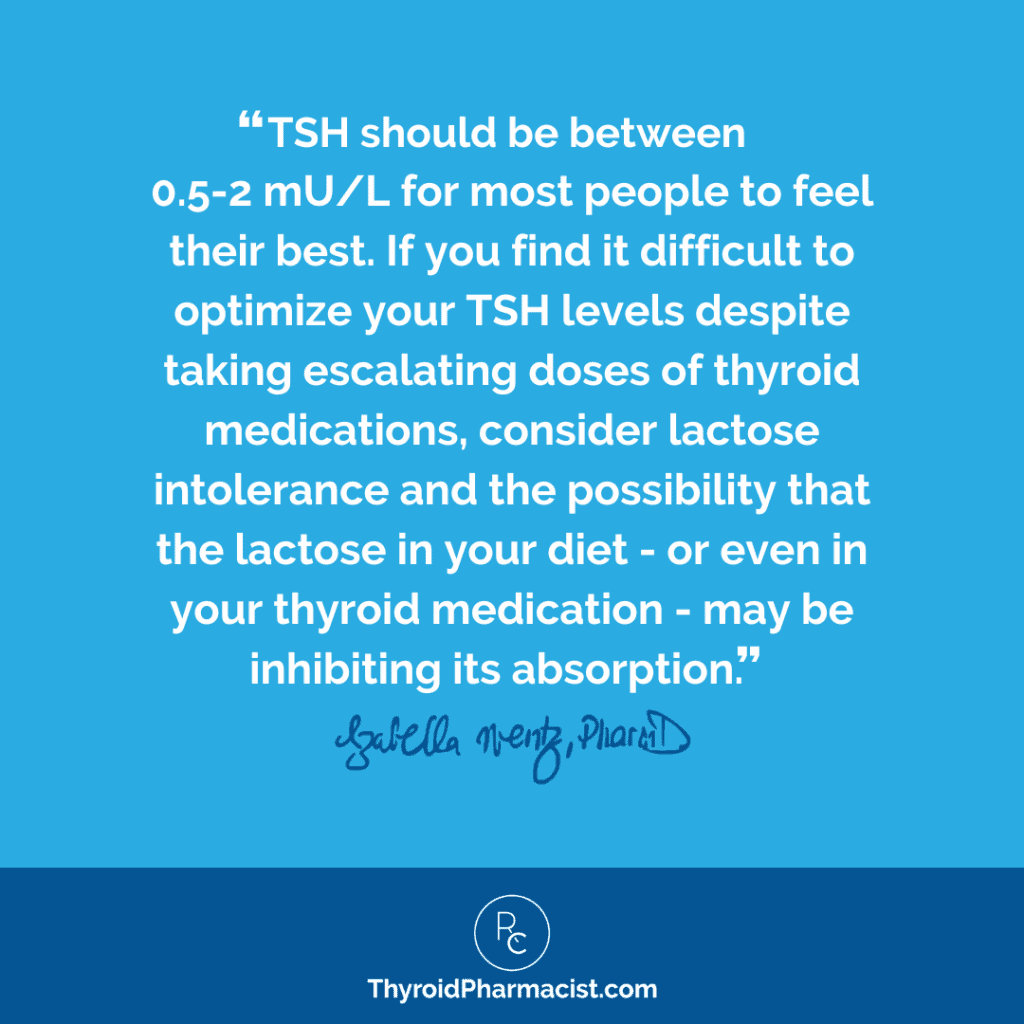
When it comes to thyroid hormones, having optimal levels is key to feeling your best.
While a TSH as high as 4 μIU/mL may be considered to be within normal limits — at least, by many conventional doctors — when my TSH was at that level, I felt like a sloth and was losing a ton of hair.
So what is considered “normal,” anyway? When scientists first set the “normal” ranges of TSH for “healthy” individuals, they inadvertently included individuals with compromised thyroid function, such as the elderly, in the calculations leading to an overly lax reference range. The range for conventional practitioners has been as broad as 0.2 to 8.0 μIU/mL, but today most conventional practitioners will consider a range of about 0.5 to 4.5 μIU/mL as normal. The problem is that you can still be hypothyroid with a TSH of below 4.5 μIU/mL.
These skewed reference ranges can result in people with underactive thyroid hormones being told that their thyroid tests are “normal”, when in fact they are anything but!
Based on recent research, the American College of Clinical Endocrinologists has defined a new and more accurate reference range to be between 0.3-3.0 μIU/mL.
For optimal thyroid function, I’ve found that a TSH between 0.5-2 μIU/L is where most people feel at their best. From the survey respondents, 69 percent said they feel optimal with a TSH under 1 μIU/mL, and 57 percent felt good with a TSH between 1 and 2 μIU/mL.
In my clinical experience, many individuals struggle with symptoms even with TSH levels considered to be normal by conventional practitioners. For this reason, I’ve written two articles which explain in detail why you could still potentially have Hashimoto’s or a thyroid condition, despite having normal TSH levels. I encourage you to check out my article on the Top 10 Thyroid Tests and my article on What If Your TSH is Normal But You Are Anything But to learn more!
Please also take a look at my article on how to get accurate lab tests for more information on different factors that can affect your lab results.
8. Low-Dose Naltrexone (LDN) Can Make a Big Difference for Some Individuals
Naltrexone, an FDA-approved medication, has traditionally been used for opioid withdrawal since the 1980s; for this purpose, it is used at a higher, standard dose of 50 mg per day.
However, low doses of this medication (hence, the name Low-Dose Naltrexone or LDN), have been found to modulate the immune system and have shown promise in improving cases of autoimmune disease such as Hashimoto’s.
Survey results showed that, while only 38 percent of those that tried LDN reported feeling better, the ones that saw benefits had some spectacular results:
- 48 percent were able to reduce thyroid antibodies
- 61 percent saw an improvement in mood
- 66 percent were able to have more energy
- 40 percent saw a reduction in pain
One reader even wrote:
“Low Dose Naltrexone changed my life for the better. If I had not added that to my regimen, I would still be suffering from nerve pain and uncontrollable allergy symptoms, in addition to the problems I have from the Hashimoto’s.”
How does LDN work to produce such great results? It balances the immune system by reducing specific immune cells called Th-17, which promote autoimmunity. This means that it turns off the cells that cause autoimmunity! It also boosts levels of endorphins, which modulate the immune system.
I recommend doses of 1.5 to 4.5 mg per day. As always, be sure to discuss with your doctor to determine if LDN is right for you and your needs.
For more information, check out my article on LDN.
9. Probiotics Can Help Normalize Weight and Improve Gut Health
Lastly, probiotics (good bacteria that help balance our gut flora) seemed to be very beneficial for many of those who took my survey.
About 75 percent said it made them feel better. Only three percent said that probiotics made them feel worse. I suspect the bad reactions were due to having SIBO, which can cause reactions to most probiotics.
Of note, 36 percent of people felt that probiotics helped them normalize their weight.
There is a confirmed link between gut health and weight. Research shows that people who are overweight have an imbalance of specific types of bacterial flora in their intestines. Those who are overweight may have particular bacteria strains that extract more calories from food compared to those found in people who are not overweight. (This means that one could be eating the same amount of food as their friends, yet gain more weight.)
Research suggests that the ratio between two probiotics, Bacteroidetes and Firmicutes, may determine one’s level of leanness. Having more Bacteroidetes than Firmicutes in your gut means you’ll likely absorb less fat and calories, and be more likely to be lean. (Interested in learning more? I’ve written an article which discusses how to use probiotics to achieve a healthy weight.)
Aside from balancing weight, probiotics have also been widely researched for a variety of conditions, including irritable bowel syndrome, constipation, anxiety, depression, and even skin disorders. They can help improve digestion and nutrient extraction from the foods we eat, and can also balance the immune system.
Additionally, probiotics can help with many types of gut disorders, including small intestinal bacterial overgrowth (SIBO), which is present in over 50 percent of people with Hashimoto’s.
Here are some of the probiotics that I recommend and that you may consider:
- Saccharomyces boulardii (S. boulardii) – This is a beneficial yeast that helps to clear out pathogenic bacteria, including Candida, Blastocystis hominis, and H. pylori. Unlike most probiotics, S. boulardii is generally well tolerated by those with SIBO.
- Rootcology ProB 50 – This contains 50 billion colony forming units of Lactobacillus and Bifidobacterium strains, and is a great high-dose probiotic to start with as you work your way up. (Unlike many high dose probiotics, ProB 50 has the benefit of being stable at room temperature.)
- Microphage – Microphage is a specialized formulation made from seven different strains of probiotics and four types of bacteriophage. They selectively target E. coli bacteria, which are implicated in SIBO, chronic UTIs, and various autoimmune conditions, including Hashimoto’s. This product uses delayed-release technology, which helps ensure delivery of active bacteriophage to the small intestine, without getting destroyed by stomach acid. When beneficial bacteria is supported in the gut, this can help to strengthen the immune system.
- Klaire Ther-Biotic – This is a less expensive but equally effective brand of high-dose multi-strain probiotics recommended by my brilliant nutritionist friend, Tom Malterre.
- Spore-Based Probiotics – Spore-based probiotics have a unique mechanism of action, which allows the spores to directly modulate the gut microbiome. Spore-based probiotics have shown promise in various autoimmune diseases and in reducing allergies and asthma. Spore-based probiotics also have an ability to boost Lactobacillus colonies, so they can be used concurrently with Lactobacillus probiotics as well as in place of them. Unlike Lactobacillus probiotics, spore-based probiotics can reduce SIBO and increase gut diversity by boosting the growth of other beneficial flora. Clients and colleagues with Hashimoto’s have reported the following after using MegaSporeBiotics for 30 to 90 days: a reduction in thyroid antibodies, improved mood, less pain, better bowel movements, more energy, and a reduction or complete elimination of food sensitivities. I have just added Spore Flora to the Rootcology portfolio, and I have also used MegaSporeBiotic with great results.
Be sure to check out this article on the benefits of probiotics to find out what may work best for you.
Here’s a message from someone who has implemented probiotics into their diet (along with many of the other interventions discussed above) and has seen a tremendous improvement:
“I was diagnosed with underactive thyroid and had radiation in 1969 as a child, Synthroid treatment for years, rheumatoid arthritis diagnosed in 2012 along with Sjogren’s syndrome, leaky gut, and chronic sinus infections. I was a weak, sick, nearly bedridden woman on a ton of medicine. I was getting sicker and being prescribed more dangerous and expensive medications with no real end in sight for pain or healing. Even with all this chaos in my body I constantly searched for answers and did my best to take care of myself, I had no idea that I was making myself sick with food and chemicals and tap water and a million other things.
I have removed as many chemicals from my life as I can, eat organic, take vitamins, minerals and probiotics, eat fermented foods, drink kefir, have reduced all stress, sleep a lot, rest a lot, go on walks, meditate, drink clean water and think peaceful thoughts. I don’t take on too much, and I play as much as I can.
In the past year, I have been able to remove all meds for rheumatoid arthritis and reduced the thyroid meds also. I am active, 40 pounds lighter and glad to be alive again. I have a way to go yet but I’m better now than I have been in years. Thank you for the work you have done and for compiling this valuable information.”
The Takeaway
I know that Hashimoto’s can make us feel very much alone, especially when no one else we know personally has the condition. Even when others we know have Hashimoto’s, the condition can manifest with different levels of severity in different individuals, making us wonder why we feel so much worse than others. I’ve been there.
I want you to know that you’re not alone and that you can get better. I’m here for you, and together, we can overcome Hashimoto’s.
Here’s a summary of the nine takeaways from those who took my survey:
- Reduce stress from a physiological and mental-emotional perspective, to further your healing.
- Address nutrient deficiencies through dietary changes, and supplement when needed.
- Find a healing diet that works best for you (and eliminate gluten if you are sensitive to it).
- Implement self-care strategies such as sauna or massage therapy.
- Ensure your TSH levels are optimal.
- Consider Low-Dose Naltrexone (LDN) if your doctor gives you the go-ahead to use it.
- Consider probiotics.
To help support you on your health journey, I’ve made the nutrient deficiencies chapter of my book Hashimoto’s: The Root Cause available for free. You can download it for free when you sign up for my weekly newsletter, here.
I’ve also written an entire book, Hashimoto’s Protocol, that uses the root cause approach and has outlined a 90-day done-for-you protocol to help put your thyroid condition into remission.
I hope this survey of interventions encourages you to take charge of your health and to find a deeper level of healing. I recommend dedicating one hour each day to self-care. I encourage you to focus on things that relax you and make you feel better, prepare nourishing foods, and stay on top of your supplements and labs. After all, what gets measured gets managed!
Give yourself the same care as you would a loved one, child, or pet who needs you.
I hope that you found this information helpful in your healing journey. Please know I am here to support you, and would love to hear from you in the comments below.
I love interacting with my readers on social media, and I encourage you to join my Facebook, Instagram, TikTok, and Pinterest community pages to stay on top of thyroid health updates and meet others who are following similar health journeys. For recipes, a FREE Thyroid Diet start guide, and notifications about upcoming events, be sure to sign up for my email list!
References
- Harvard Health Publishing. Understanding the stress response. Harvard Health Publishing. https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response. Published March 2011. Updated March 18, 2016. Accessed February 25, 2018.
- Vitamin B12. Therapeutic Research Center website. https://naturalmedicines-therapeuticresearch-com.mwu.idm.oclc.org/databases/food,-herbs-supplements/professional.aspx?productid=926. Updated March 7, 2018. Accessed March 22, 2018.
- Ness-Abramof R, Nabriski DA, Braverman LE, Shilo L, Weiss E, Reshef T, et al. Prevalence and evaluation of B12 deficiency in patients with autoimmune thyroid disease. Am J Med Sci. 2006 Sep;332(3):119-22.
- Tamer G, Arik S, Tamer I, Coksert D. Relative vitamin D insufficiency in Hashimoto’s thyroiditis. Thyroid. 2011;21(8):891-896. doi:10.1089/thy.2009.0200.
- Wang J, Lv S, Chen G, et al. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients. 2015;7(4):2485-2498. doi:10.3390/nu7042485.
- Eftekhari MH, Keshavarz SA, Jalali M, Elguero E, Eshraghian MR, Simondon KB. The relationship between iron status and thyroid hormone concentration in iron-deficient adolescent Iranian girls. Asia Pac J Clin Nutr. 2006;15(1):50-55.
- Hyman M. How Good Gut Health Can Boost Your Immune System. EcoWatch. 2015. https://www.ecowatch.com/how-good-gut-health-can-boost-your-immune-system-1882013643.html. Accessed January 15, 2018.
- Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature. 2009;457(7228):480-484. doi:10.1038/nature07540.
- Why the Sellers of VSL#3®* Were Found Liable for False Advertising. Visbiome website. https://www.visbiome.com/pages/vsl-3-story. Accessed December 9, 2020.
- Naiyer AJ, Shah J, Hernandez L, et al. Tissue transglutaminase antibodies in individuals with celiac disease bind to thyroid follicles and extracellular matrix and may contribute to thyroid dysfunction. Thyroid. 2008;18(11):1171-1178. doi:10.1089/thy.2008.0110
- Krysiak R, Szkróbka W, Okopień B. The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Drug-Naïve Women with Hashimoto’s Thyroiditis: A Pilot Study. Exp Clin Endocrinol Diabetes. 2019;127(7):417-422. doi:10.1055/a-0653-7108
Originally published in June 2015, this article has been revised and updated for accuracy and thoroughness.