I often get asked if there is one thing that people with Hashimoto’s should do right away to feel better. My answer is always, “There are two! Get off gluten and balance your blood sugar levels!”
Balancing blood sugar levels should be one of the top priorities for anyone who is hoping to overcome autoimmune thyroiditis (and adrenal fatigue). It was one of the first interventions I tried when working to heal my own thyroid condition, and it made a big difference for me.
I wasn’t aware that I had blood sugar issues when I was first diagnosed (despite being a self-admitted sugar addict). I was thin — therefore, I assumed that I was healthy. However, I would get “hangry” (hungry + angry) multiple times per day, as the high carbohydrate foods I had consumed were causing me to experience huge blood sugar swings. What I didn’t know was that these swings were also weakening my adrenals and causing a spike in my thyroid antibodies.
In this article, I’d like to dig a bit deeper into answering questions about blood sugar, including:
- What are blood sugar imbalances?
- How do blood sugar imbalances impact Hashimoto’s?
- How can you control blood sugar levels without medications?
- What are some tips to naturally reduce blood sugar levels today?
What are Blood Sugar Imbalances?
Blood sugar, also called glucose, is the primary sugar that enters the body through the foods that we eat. As an energy source for the body, it provides nutrients to the organs, muscles, and nervous system.
Glucose enters the bloodstream through the small intestine after carbohydrates are consumed. The pancreas then produces insulin to help keep blood sugar levels in check, converting excess glucose to glycogen, and sending it to the liver for storage.
Blood sugar imbalances occur when our blood sugar swings out of a normal, steady range, usually from consuming high carbohydrate foods that spike blood sugar levels before they drop quickly, like a rollercoaster.
When we consume large amounts of sugar — often in the form of high carbohydrate foods such as desserts, grains, and starchy vegetables — the pancreas has to release larger amounts of insulin to bring the levels of sugar in the blood back down. These surges in insulin can cause blood sugar levels to drop too low, which then causes cravings for more carbohydrate-rich foods. This starts the cycle all over again as blood sugar levels swing high and low, creating stress in the body.
Common symptoms of blood sugar levels that are out of balance include hormonal issues, fatigue, depression, anxiety, insomnia, poor brain function, and chronic pain. (1-5)
In my experience, these symptoms are sadly all too common in our society, and I believe that a part of the reason for this, is that processed carbohydrates have been at the base of the Food Pyramid for decades. Fortunately, the new USDA MyPlate no longer encourages people to eat the equivalent of one bread loaf’s worth of carbohydrates on a daily basis!
I still think that there is too much of an emphasis on carbohydrates in mainstream culture despite the fact that they are actually the one macronutrient that is not required for survival!
How Do Blood Sugar Imbalances Affect Hashimoto’s?
Research has shown that up to 50 percent of those with Hashimoto’s have a carbohydrate intolerance. (6) This means that when a high-carbohydrate meal is consumed, our blood sugar levels are more likely to spike quickly, leading to low blood sugar levels (reactive hypoglycemia), as well as feelings of nervousness, lightheadedness, anxiety, and fatigue.
Blood sugar imbalances have been described as adding “fuel to the fire” in autoimmune thyroid disease, by many practitioners who focus on reversing Hashimoto’s.
Blood sugar levels and the thyroid are intimately connected. A review paper published in 2010 that discussed the relationship between thyroid dysfunction and metabolic disorders, highlighted the fact that patients with diabetes were up to three times more likely to develop a thyroid disorder. (7)
This correlation is due in large part to the fact that increased stress on the body can cause damage to the thyroid. When blood sugar levels are constantly fluctuating, the body experiences these changes as chronic stress. When the adrenals (the glands that are responsible for releasing stress hormones) become stressed, they release an excess of the hormone cortisol, which can also lead to an increased production of inflammatory proteins that are associated with a heightened immune response. This pattern eventually leads to an altered release of cortisol, which can lead to numerous symptoms including chronic fatigue, mood swings, and increased thyroid antibodies. (Weakened adrenals can also weaken the thyroid!) (8-11)
I recommend working to stabilize your blood sugar to help protect your adrenals from excess stress and heal from hypothyroidism. Many of my clients have reported improvements in mood, energy, brain function, and weight after balancing their blood sugar and improving their adrenal function!
How Do You Know If Your Blood Sugar is Out of Balance?
My blood sugar was around 50 mg/dL (very low), right before I got diagnosed with Hashimoto’s. I often used to feel lightheaded, faint, and anxious, without knowing why.
If you’ve been diagnosed with diabetes or prediabetes, you’ll likely know that your blood sugar is out of balance. If you have Hashimoto’s, blood sugar abnormalities are extremely common, and many people with Hashimoto’s will present with hypoglycemia (low blood sugar) in the early stages. (12)
Hypoglycemia is an early risk factor for developing diabetes. It also exacerbates Hashimoto’s and other autoimmune conditions.
Here are some symptoms of low and high blood sugar. Please note that these are generalized lists of symptoms that are meant to help you address day-to-day changes in blood sugar levels and help you stabilize swings in blood sugar. However, they are also symptoms of diabetes. If you have ongoing and/or severe symptoms of this nature but have not yet been diagnosed with diabetes, please see your practitioner as soon as possible to get tested.
Symptoms of low blood sugar levels include: (4,13,14)
- Craving sugary foods
- Irritability and lightheadedness if meals are missed, A.K.A. feeling “hangry”
- Dependency on caffeine
- Needing food to relieve fatigue
- Shaky, jittery, or tremulous feelings
- Nervousness or agitation
- Forgetfulness
- Blurred vision
- Mental fog
- Cold extremities
Symptoms of elevated blood sugar levels include:
- Fatigue, after meals and in general
- Persistent hunger
- Cravings for sugary foods that are not eliminated after eating them
- Needing desserts after meals
- Waist girth equal to or larger than hip girth
- Frequent urination
- Increased appetite and thirst
- Difficulty losing weight
Testing for Reactive Hypoglycemia
If you tend to have dramatic blood sugar swings simply after eating, you may be experiencing reactive hypoglycemia. Reactive hypoglycemia is an abnormal reaction of excess insulin secretion in response to eating (typically characterized as a “sugar crash” caused by a quick spike then drop in insulin). With reactive hypoglycemia, unusual insulin patterns can continue even after the meal is digested.
This can happen after eating high carbohydrate meals, but some individuals may have a hypoglycemic response to low carbohydrate foods as well. Drops in blood sugar usually occur one to four hours after eating.
If blood sugar levels drop below 70 mg/dL during this four-hour period, this could be an indication that you are experiencing reactive hypoglycemia.
Symptoms are similar to those of low blood sugar as listed above, and may also include:
- Sleeping problems
- Heart palpitations
- Fatigue
- Sweating/hot flashes
- Headaches
- Depression
- Flushing or paleness
- Increased appetite
- Nausea, vomiting
- Panic attack
- Hot flashes
- Anxiety
- Trouble talking
- Disorientation
As mentioned above, low blood sugar is common in those with hypothyroidism, and so is reactive hypoglycemia. Interestingly, H. pylori can be a trigger for both. (12,15-19)
You can easily test yourself for reactive hypoglycemia with the use of an over-the-counter blood glucose monitoring kit, which uses a small finger prick to collect a sample of your blood. Follow these instructions to test your reactions:
- After at least 10 hours of fasting (such as first thing in the morning), test your blood sugar before eating your first meal of the day.
- Eat a meal with your typical carbohydrate serving.
- Record the meal in a journal.
- Repeat testing every 30 minutes, for a total of four hours.
- Repeat as necessary to test other foods.
Another great tool to monitor blood sugar levels is a continuous glucose monitor (CGM). This is a small sensor that you apply to the back of your arm. It measures and stores your glucose readings throughout the day, which you can access through an app on your phone. If you’re looking to get a big picture overview of your blood sugar levels and how different foods affect them, a CGM is a great option. It also eliminates the hassle of constantly pricking your finger for readings.
A surprising thing I’ve learned over the years is that different foods may produce different reactions. I suspect this is largely connected to our unique mix of genetics, health conditions, microbial balance, digestive enzymes, and nutrients that determine how we “process” each unique food molecule.
Factors That May Affect Blood Sugar Imbalance
You may be at a higher risk for blood sugar imbalances if you have certain co-existing conditions, including the following:
Metabolic Syndrome
Metabolic syndrome is a group of symptoms that increase one’s risk of cardiovascular disease, stroke, and type 2 diabetes. (20)
Metabolic syndrome can be diagnosed when three or more factors are present:
- Low high-density lipoprotein (HDL) levels
- Abdominal obesity (with fat gain in the midsection)
- Insulin resistance (high fasting glucose)
- High blood pressure
- High triglycerides
Additionally, although not required for a formal diagnosis, I have observed a proinflammatory state with metabolic syndrome. This is due to the increased adipose tissue (from increased fat in the midsection). Adipose tissues release a baseline amount of inflammatory substances. Thus, the more adipose tissue there is, the more inflammation is present.
Note: If a person has just one of the diagnoses from the list above, it does not mean that they have Metabolic Syndrome. However, it does increase their risk of being diagnosed with Metabolic Syndrome.
Type 2 Diabetes
Diabetes occurs when the body does not produce or respond to insulin — the hormone that regulates blood sugar. In type 2 diabetes, cells within the body have a reduced response to insulin. Blood sugar (blood glucose) is the body’s primary fuel source and enters the bloodstream through the small intestine, after carbohydrates are consumed. Without the proper dose of insulin, the body’s blood glucose levels remain elevated and, over time, create a cascade of symptoms in the body, such as heart attack, stroke, and kidney damage, that can become life-threatening.
Polycystic Ovarian Syndrome (PCOS)
Polycystic Ovarian Syndrome, or PCOS (in females), is often diagnosed by two of the three following criteria: hyperandrogenism (excess androgen hormones), ovulatory dysfunction, and cystic ovaries. Often it is a diagnosis of exclusion, which means other related conditions have to be ruled out before giving a diagnosis of PCOS. PCOS causes symptoms such as: (21,22)
- Irregular menstrual cycles
- Insulin resistance
- Hirsutism (hair in certain places, such as on the face)
- Acne
- Male pattern baldness (in women)
- Anovulation
The Gut Microbiome
From a functional medicine perspective, over the last decade, I have learned about our diet, as well as our microbiome, nutrient status, and toxic load, as contributors to blood sugar balances. I will discuss foods and nutrients in the section below, but I wanted to touch on a few important potential root causes that can be the drivers behind both Hashimoto’s and blood sugar issues.
Our gut microbiome is a powerful body system. Studies have shown that the composition of our gut’s inhabitants can determine our nutrient status as well as how much and which types of calories we extract from our environment. Additionally, our microbiome can impact our blood sugar levels. (23,24)
I used to think that sugar was the root cause, because high sugar diets made us more susceptible to gut infections like Candida. Recent research suggests that this is true; it has been demonstrated by various studies in people with diabetes — the high sugar environment encourages an overgrowth of yeasts and molds. (25)
However, my experience and recent research suggest that gut infections/colonizations themselves can contribute to blood sugar issues. The three in particular I have been finding include:
- Candida – While we all have Candida albicans in our gut flora in varying amounts, it can become a problem when there is an imbalance between Candida and other microorganisms in the body. When this happens, Candida is considered a pathogenic infection. Aside from digestive symptoms, a Candida infection can also impact insulin levels. One study showed that Candida can provoke an elevated level of insulin secretion, which increases one’s risk of developing diabetes. (26)
- H. pylori – Helicobacter pylori (H. pylori) is also a gut infection that can be a trigger for Hashimoto’s. It burrows into our stomach lining and secretes urease, which neutralizes stomach acid. This byproduct is toxic to epithelial cells (cells lining the surface of the gut), which leads to damaged cells, a disruption of tight junctions, and inflammation. It has also been shown that those with H. pylori often experience hypoglycemia symptoms, which is when one’s blood sugar dips too low, resulting in potential symptoms like lightheadedness, brain fog, and shakiness. One study followed 12 people with H. pylori and measured their post-meal serum insulin responses, post-meal plasma glucose levels, and the number and severity of postprandial symptomatic hypoglycemic (PSH) attacks, before and after treatment of H. pylori. Researchers found that insulin responses and post-meal glucose decreased significantly after eradicating the infection. They also followed the patients for one month after treatment, and found that the number and severity score of PSH attacks decreased significantly. (27)
- Mold toxicity – Upon doing a quick search, I didn’t find any studies that show that mold toxicity can lead to blood sugar issues, but I have seen it clinically. In my years of functional medicine training and conversations and consultations with brilliant colleagues, I have also learned that Candida tends to overgrow when the opportunity arises, and mold creates the right environment for Candida, so there certainly can be a link. In my experience, H. pylori overgrowth is also commonly present in people with mold toxicity.
Control Blood Sugar Levels Naturally
In my experience, most people with Hashimoto’s and blood sugar imbalances (who have not been diagnosed with diabetes and do not have severe symptoms) can stabilize their blood sugar with simple diet and lifestyle changes and won’t have to use medications, as can be the case when blood sugar issues progress to insulin resistance and diabetes. Those with diabetes can also benefit from lifestyle changes, but may need a more intensive functional medicine plan that is beyond the scope of this article, to get in balance. 😉
Lifestyle Changes to Balance Blood Sugar Levels
1. Exercise. Regular exercise helps the body’s cells become more sensitive to insulin, which can help us avoid insulin resistance and reduce thyroid symptoms. Glucose is the primary fuel source for our muscles, and when we engage in moderate exercise, such as walking, our muscles pull more glucose from our blood. Additionally, our cells become more responsive to insulin by increasing receptors, allowing more glucose to enter the cells rather than staying within the blood. Over time, these changes can lower our blood sugar levels. (28)
Exercise can help to balance cortisol and blood sugar levels; however, for those with hypoglycemia, it’s important to be careful when it comes to strenuous exercise, as it can worsen or even cause hypoglycemic reactions. Strenuous exercise can cause the body to produce more cortisol — which in turn can raise blood sugar levels. (29,30) So if you tend to feel worse after exercise, this could be why.
If you are concerned about imbalanced blood sugar levels, I recommend going easy with your exercise routine. In order to avoid a hypoglycemic reaction, as well as to work on getting blood sugar and cortisol in balance, I suggest gentle exercises like walking, swimming, and yoga. These are all great ways to incorporate more exercise into your day without adding more stress to your body.
2. Hydration. Drinking enough water may help keep blood sugar levels balanced, by helping your kidneys flush out excess blood sugar through your urine. Keep in mind that water and other non-caloric beverages are best, while sugar-sweetened drinks raise blood glucose levels. Adding in some electrolytes, such as Rootcology Electrolyte Blend, a complete and balanced electrolyte formula, can also help ensure your body is well hydrated.
A study done on healthy adults with blood sugar levels within a normal range, found that as water intake increased, the risk of developing hyperglycemia (high blood sugar) decreased. (31) In my clinical experience, I’ve also seen dehydration linked to adrenal issues. So, the simple act of hydrating can have a twofold effect of helping to balance adrenals and blood sugar!
Aim for half your body weight in ounces per day – so a 150-pound person would drink at least 75 oz. of water per day.
3. Sleep. Getting enough quality sleep is important for blood sugar balance and insulin sensitivity. A lack of sleep affects metabolic hormones, including growth hormone (somatotropin), and raises cortisol levels. These hormonal imbalances can disrupt insulin levels, while also increasing appetite and cravings for carbohydrate-laden foods that will further increase blood sugar swings. (32)
Balancing Blood Sugar Levels with Diet
Focusing on the impact of food on our blood sugar is the most effective way to balance our blood sugar levels, and this is best accomplished by paying close attention to the glycemic index of foods. (33)
The glycemic index is a measure of how quickly food becomes assimilated into our bodies. It can also be referred to as the “burn” rate — how quickly we burn the fuel we receive from these foods. Focusing on low glycemic index (GI) and low glycemic-loaded (GL) foods, which burn slower, can really help with balancing blood sugars.
Foods with a glycemic index of less than 55 are considered to have a low glycemic index. These include most non-starchy vegetables, meats, nuts, seeds, and some whole grains. Fruits with less fructose (“sour” fruits such as grapefruit, lemons, limes, and cranberries) also have a low glycemic index.
Foods with a glycemic index above 55 are considered high glycemic index foods and include processed grains, sugar, starchy vegetables like potatoes, and sweet fruits like watermelon.
The glycemic index of foods can be referenced at glycemicindex.com.
The graphic below gives you an idea of how high and low GI foods affect blood sugar over a two-hour period. As you can see, high GI foods spike blood sugar levels high, which crash dramatically after 30 minutes have passed. Low GI foods, however, produce a smaller spike that declines relatively slowly.
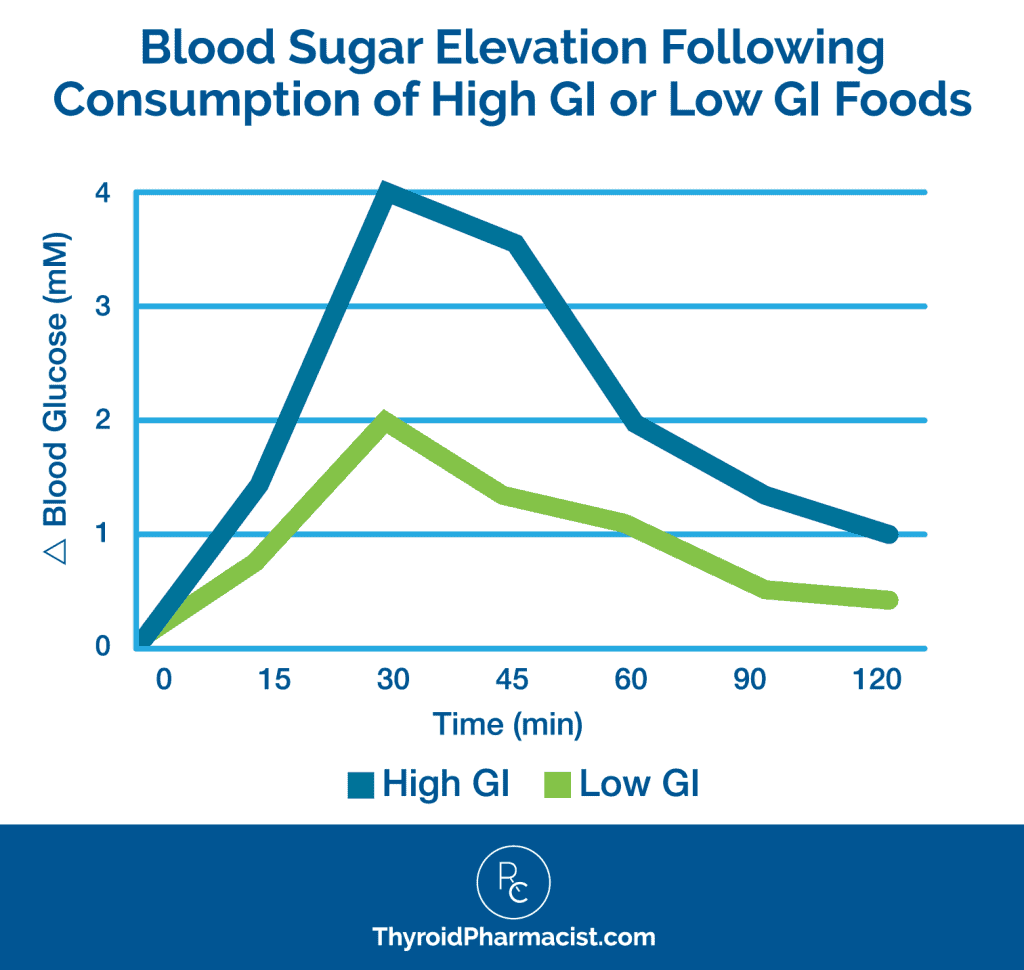
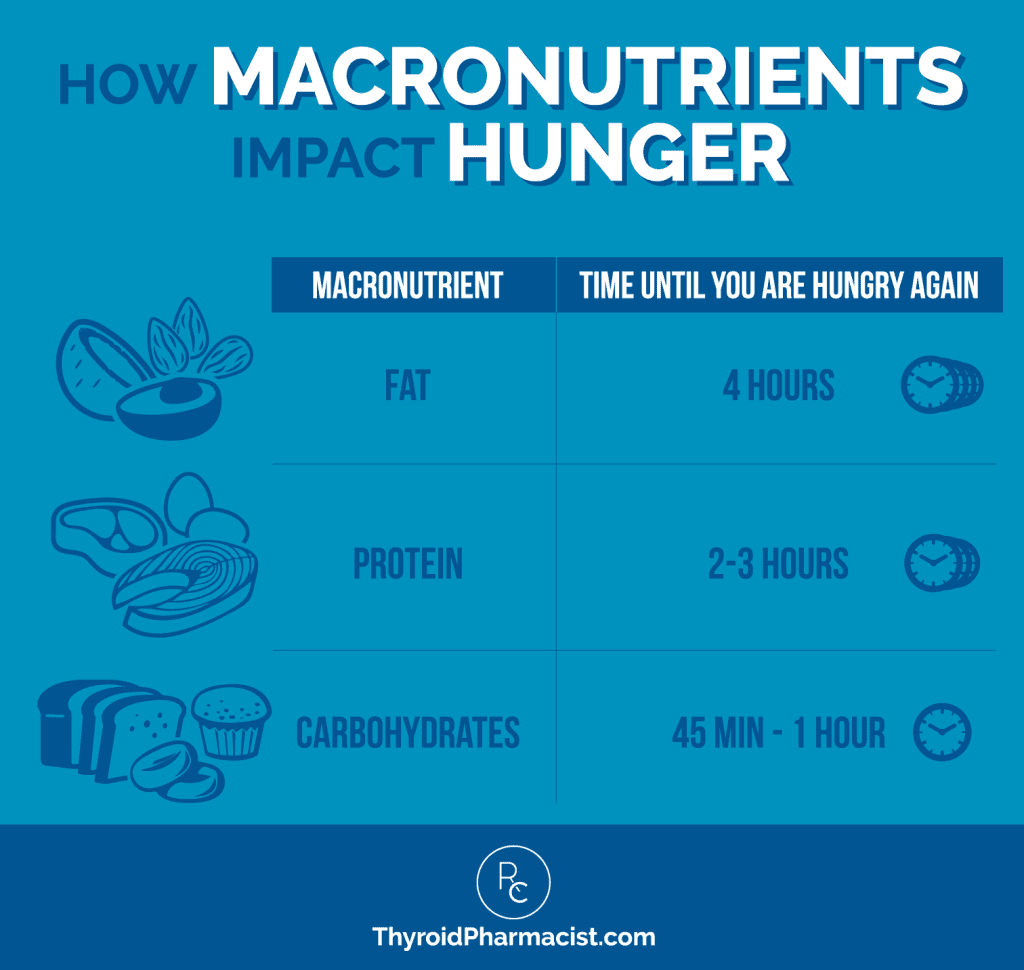
Carbohydrates have a very fast burn rate and can spike blood sugar levels dramatically. Since they can quickly become assimilated into our bodies, we may feel hungry again less than an hour after eating them.
Instead of loading up on carbs, I recommend increasing your intake of (healthy) fats and proteins, as they have a slower burn rate and become assimilated into our bodies in a slower and more gradual manner. A person will be hungry again two to three hours after eating protein, and four hours after eating fat.
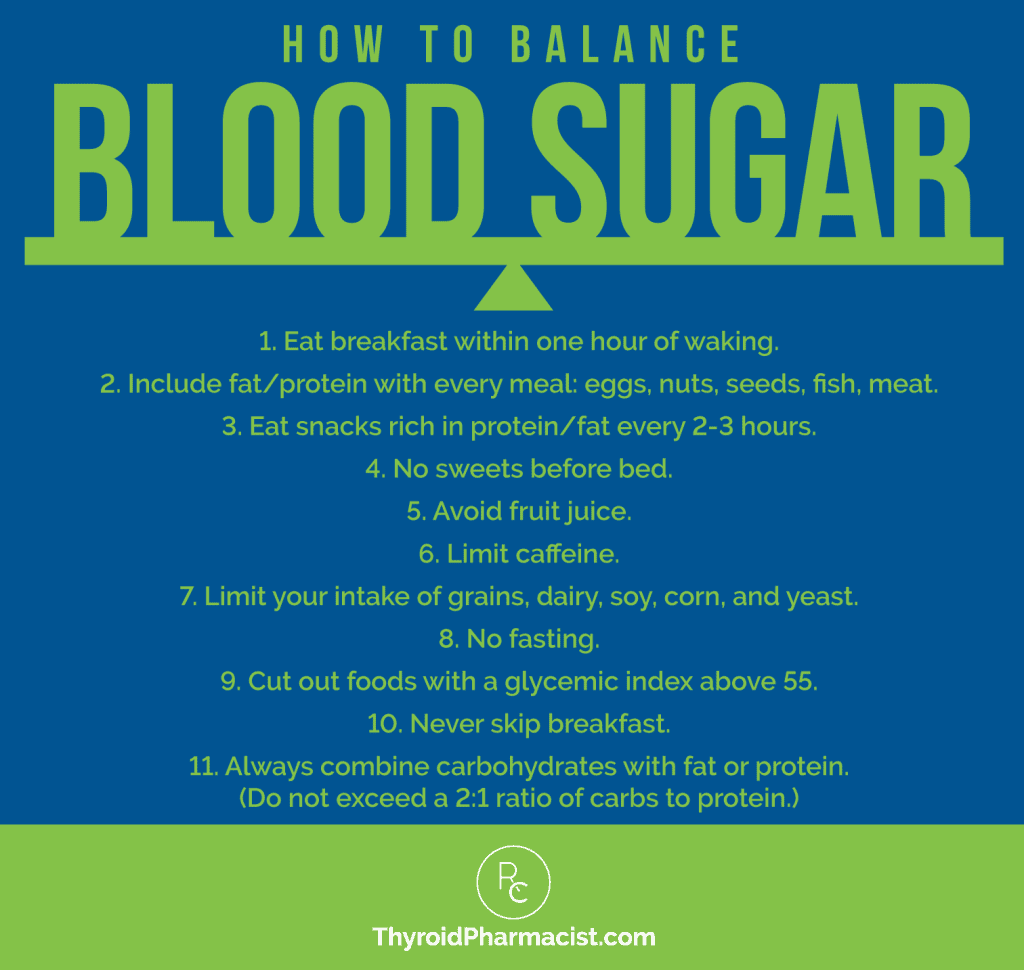
The following quick reference can be printed out to make balancing your blood sugar much easier:
Another important thing to note is that combining carbohydrates with protein can slow down the glycemic impact of the carbohydrates you consume. If you do consume some carbohydrates, I recommend a ratio of no larger than two servings of carbohydrates to one serving of protein. (For example, if you are having four ounces of steak, you should have a maximum of eight ounces of potatoes.)
Eating a low glycemic index diet that is low in carbohydrates helps with feeling fuller longer, improves cholesterol and blood sugar levels, improves cognitive performance, improves energy, and reduces acne. It also reduces the risk of developing diabetes, heart disease, and some cancers, while promoting weight loss for those who are overweight. (34-36)
Of the people with Hashimoto’s who took my 2015 survey, 61 percent reported an improved mood, 71 percent had better energy, and 53 percent experienced weight loss on a low GI diet!
Other Tips For Balancing Blood Sugar with Diet
Are you ready to begin addressing your blood sugar levels? There are a few important dietary rules to keep in mind that will help keep them balanced throughout the day:
1. Include fat and protein with every meal — good sources include eggs, nuts, seeds, fish, and meat. Protein powders are another great way to get protein in your diet! You can read about the safest protein powders for Hashimoto’s here.
2. Eat every two to three hours. Small, low-carb snacks between meals and before bed can help stabilize blood sugar levels and manage Hashimoto’s symptoms. (Snacks rich in protein and fat are great. Green smoothies made with Organic Pea Protein Powder or Hydrolyzed Beef Protein from Rootcology are my favorite!)
Note: For my Hashimoto’s clients, I typically recommend eating less frequently to address SIBO (a potential causal factor in Hashimoto’s) to allow the migrating motor complex (MMC) to work at clearing out microbes from our small intestine. However, in the early stages of blood sugar balance, we will need to eat snacks every two to three hours. Once you address the blood sugar issues (and potential underlying causes of SIBO like H. pylori), you may be able to stretch out the time between meals to allow for the MMC to work.
3. Do not eat sweets less than three hours before bed to avoid blood sugar swings that can elevate stress hormones and prevent sleep.
4. Avoid fruit juice on its own, as most fruit juices are loaded with quick-burning sugar.
5. Limit your intake of caffeine, as caffeine stimulates the adrenals to get stress hormones to bring blood sugar back up, which in turn creates a cycle of imbalance. You can read more about caffeine and Hashimoto’s here.
6. Limit grains and avoid all gluten, dairy, soy, corn, and yeast, as these foods are generally high in carbohydrates. I have found that they are common food sensitivities for many people with Hashimoto’s.
7. Never skip breakfast. Eat breakfast within one hour of waking (but not within 30 minutes of taking thyroid medications if you take them in the morning).
8. Always combine carbohydrates with fat and/or protein. Never exceed a 2:1 ratio of protein to carbs. In other words, aim for more protein and fewer carbs.
Addressing Nutrient Deficiencies
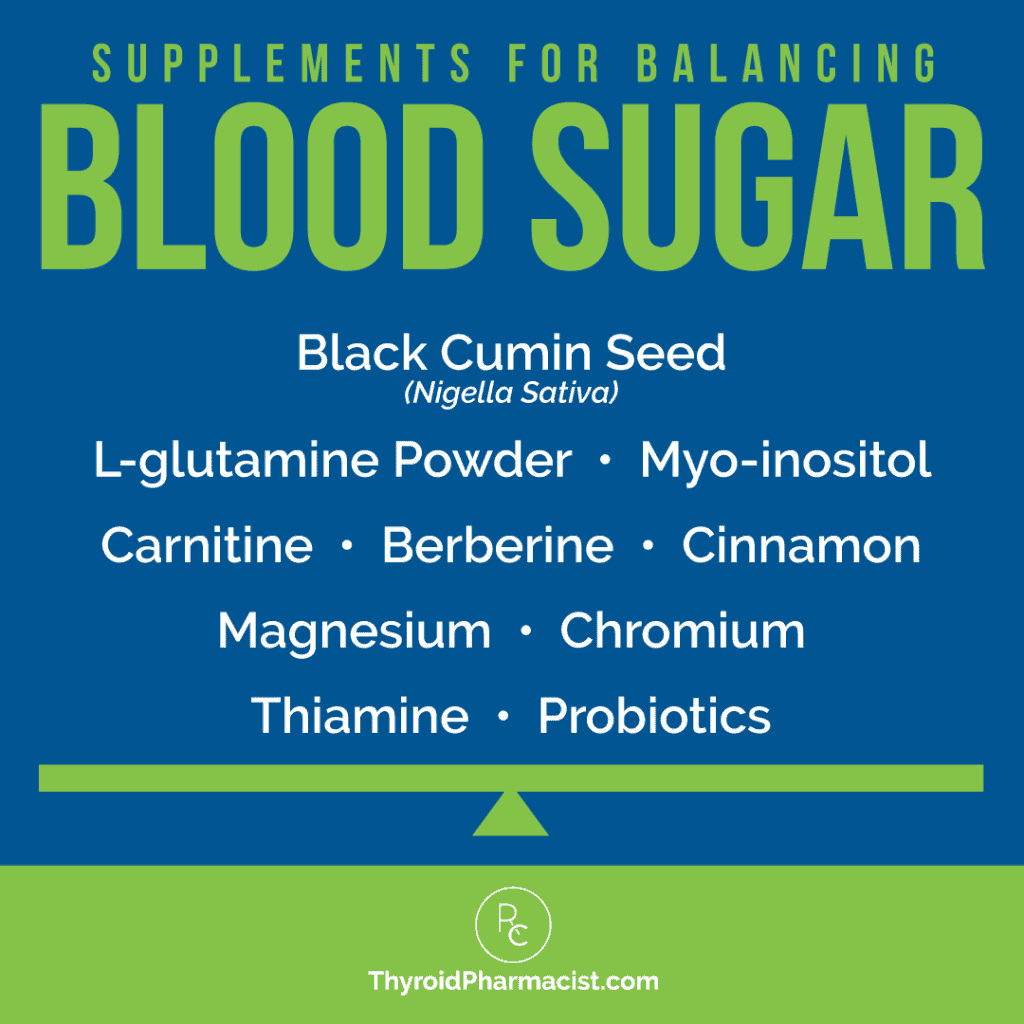
- Magnesium: Nutrient deficiencies have been shown to contribute to blood sugar imbalances, and magnesium deficiency has been linked to a higher risk of developing diabetes. One study suggested that those with the highest levels of magnesium intake had a 47 percent lower risk of becoming diabetic. (37) Thus, supplementing with magnesium may help stabilize blood sugar levels.
- Chromium: The mineral chromium is involved in carb and fat metabolism, and also helps control blood sugar levels. A lack of chromium may make one more intolerant to carbohydrates, so it’s important to boost one’s intake of foods high in chromium. (38) Such foods include egg yolks, coffee, nuts, green beans, broccoli, and meat. Additionally, I recommend supplementing with ChromeMate GTF. In my experience and through researching sleep issues for clients, I came across a certain insomnia pattern that has been tied to chromium deficiency – waking up between 2 and 3 am on days when not enough calories are consumed can be an indication of chromium deficiency. (39)
- Thiamine: Thiamine is one of the B vitamins, known as B1. Its main responsibility is to convert carbohydrates into energy, and it also helps with the digestion of proteins and fats. (40) Food sources of thiamine include fortified grains, beef liver and pork, milk (dried and fresh), eggs, legumes and peas, nuts, and seeds. Most of these foods are restricted on the Paleo and Autoimmune Paleo diets, and many people with Hashimoto’s find themselves deficient and less able to break down carbohydrates for absorption. For this reason, I recommend BenfoMax by Pure Encapsulations.
- Carnitine: Carnitine is an amino acid that is naturally produced in the body. It helps transport fatty acids into the mitochondria, where they can be burned up and used as fuel. Studies in both humans and animals have shown that carnitine supplementation resulted in an improvement of glucose tolerance, in particular during insulin-resistant states. (41) Carnitine deficiency is linked to fatigue, brain fog, constipation, digestive issues, and muscle weakness, and is common in people with Hashimoto’s (you can read more about carnitine deficiency in the linked article). I recommend Rootcology’s Carnitine Blend, which also contains the acetyl-L-carnitine form, for its unique properties in supporting brain function and reducing mental fatigue.
- Dimethylglycine: Dimethylglycine (also known as betaine) deficiency has been suggested to be a potential cause of blood sugar issues that may lead to diabetes. Supplementing with dimethylglycine may be helpful for addressing fasting blood glucose levels and may help with nutrient extraction. My favorite way to supplement with dimethylglycine is to use Betaine with Pepsin to help with protein digestion and nutrient extraction. (42-44)
- Myo-inositol: Researchers have found that this important form of inositol (a type of natural sugar alcohol), which is made in our bodies, can reduce insulin resistance often associated with polycystic ovary syndrome (PCOS). (Interestingly, PCOS often co-occurs with hypothyroidism — perhaps due to both conditions sharing blood sugar imbalances and deficiencies in myo-inositol as root causes.) A 2013 study showed supplementation with myo-inositol and D-chiro-inositol led to a significant improvement in insulin sensitivity in those with PCOS. A follow-up study in 2014 showed that the myo-inositol isoform specifically improves the metabolic profile of individuals with PCOS. Additionally, research has illustrated that myo-inositol can be helpful for gestational diabetes. (18,45-49) You can read more in my article about myo-inositol supplementation for blood sugar balancing, as well as its multiple benefits for Hashimoto’s.
- Glutamine: Used to treat diabetes and curb carbohydrate cravings, this essential amino acid helps suppress insulin levels and stabilize blood glucose. There is a known link between Hashimoto’s and type 2 diabetes, with up to 30 percent of those with Hashimoto’s developing the condition. Interestingly, research has shown glutamine to be effective in restoring insulin response in diabetics, so glutamine supplementation may be helpful in addressing blood sugar issues in those with Hashimoto’s as well. (50,51) You can find glutamine in the form of L-glutamine in bone broth, as well as in supplements like L-Glutamine Powder by Pure Encapsulations.
- Vitamin C: A recent study found that taking 500 mg of vitamin C twice daily, can help those with type 2 diabetes, by lowering elevated blood sugar levels throughout the day and reducing spikes in blood sugar after meals. (52)
- Vitamin D: Vitamin D deficiency is common in those with type 2 diabetes, and studies hypothesize that vitamin D is related to the action of insulin. A study conducted in 2012-2013 showed a decrease in HBA1c (average blood sugar) levels in those who took 4000 IU of vitamin D daily, compared to the group that took a placebo. (53) That’s why it’s important to optimize your levels of this vital “sunshine vitamin” so that your vitamin D levels fall within the optimal range of 60 to 80 ng/mL.
- Zinc: Zinc is crucial to the process of synthesizing, storing, and secreting insulin. It helps to protect the B-cells in the pancreas from damage, and has even been studied for its ability to affect the expression of genes that are linked to diabetes. (54,55)
Additionally, there are a few herbs, spices, and supplements that can be used in conjunction with a proper diet, to help stabilize blood sugar levels. I am going to list them in the order that I would typically recommend them.
- Berberine: This plant alkaloid is known to support blood sugar metabolism and normal insulin sensitivity. Studies have shown that one gram of berberine per day lowered fasting blood sugar by 20 percent in people with diabetes, which is comparable to a commonly prescribed diabetes medication. (56)
I first heard about berberine when I started going to various functional medicine conferences, and a few of the practitioners I met reported having success with lowering thyroid antibodies and thyroid symptoms with berberine. This plant has an interesting profile, as in addition to balancing blood sugar, it can be helpful in addressing gut issues such as SIBO, mold, and H. pylori (three potential root causes of Hashimoto’s).
I haven’t seen any studies of using berberine to reduce thyroid antibodies yet; however, interestingly, metformin, a drug with similar actions on blood sugar, has recently been studied in Hashimoto’s, and has shown to have the ability to reduce thyroid antibodies! (57)
Personally, berberine helped me get rid of my awful chin hairs! Because of its multitasking benefits, I recently added Rootcology’s Berberine to the Rootcology product line, and I’ve also recommended Candibactin BR to clients with excellent results.
- Resistant Starch: As the name implies, resistant starch (RS) is a type of carbohydrate that resists digestion. It’s not digested in the small intestine and moves on to the large intestine, where it’s fermented. These fermented fibers act as a prebiotic – food for the good bacteria in your gut. In addition to being an ally for your gut health, RS supports healthy blood sugar levels and insulin metabolism. (58,59) This makes it great to incorporate when working to balance your blood sugar levels.
You can find RS in foods like plantains, green bananas, chickpeas, and lentils. Cooked and cooled potatoes and rice also contain high amounts of RS.
I formulated Rootcology’s Paleo Starch so that you can reap the blood sugar and insulin-supporting benefits of RS in an easy-to-use powder. Note that this supplement contains potato starch and green banana flour, which will work for those following the Root Cause Intro Diet or the Root Cause Paleo Diet. However, since potatoes are nightshades, this supplement would not be compliant with the Root Cause Autoimmune Diet.
- Cinnamon: Studies have shown that cinnamon can lower blood sugar levels by up to 29 percent. Furthermore, cinnamon can be helpful for both type 1 and 2 diabetes. (60) It slows the rate of carbohydrate breakdown in the digestive tract and moderates rises in blood sugar levels. I also recommend pumpkin pie spice (a blend of ground cinnamon, nutmeg, ginger, cloves, and allspice) as a tasty ingredient to stabilize blood sugar. You can add it to your smoothies, gluten-free baked goods, and even hot beverages!
- Black Cumin Seed (Nigella sativa): This spice (which can be used as a seasoning for food) has been used for medicinal purposes for thousands of years. Studies have shown that black cumin seeds may lower blood sugar levels by stimulating the release of insulin from the pancreas and raising glucose absorption by muscular tissue. Diabetes patients in one recent study lowered their fasting glucose levels after consuming 2 grams of black cumin seed every day, for four to six weeks. (61) It can be taken in powder (seed) or liquid form and added to a smoothie, or as a supplement in pill form.
- Aloe: Several studies have shown that aloe vera gel, taken orally twice per day, can decrease fasting glucose levels in those with type 2 diabetes. (62) A high-grade aloe supplement, like Rootcology Aloe, taken once per day, at 500 mg, will ensure that you are getting adequate amounts of the beneficial properties of aloe. (Please note: supplements that contain the outer leaf may cause issues such as diarrhea and electrolyte loss due to its laxative effect.) See my article on aloe for more information and supplement warnings.
- Probiotics: New research has highlighted the importance of gut health for blood sugar balance, and some gut bacteria have been found to be closely linked with diabetes. (63) Thus, taking a high-quality probiotic may help nurture the gut and help stabilize blood sugar levels.
- Glutathione and Cysteine: Glutathione, an antioxidant composed of amino acids, protects B-cells (immune cells) in the body, which are particularly sensitive to oxidative stress. Type 2 diabetics typically have lowered antioxidants, and supplementing with the glutathione precursor cysteine helps restore antioxidant status. (64)
- Milk Thistle: Silymarin (one of the compounds in milk thistle) may be therapeutic in metabolic syndrome (insulin resistance syndrome) in its potential to improve insulin sensitivity and decrease blood sugar. A recent analysis found that people routinely taking silymarin saw a significant reduction in their fasting blood sugar levels. (65) The antioxidant and anti-inflammatory properties of milk thistle may also be useful for reducing the risk of developing diabetic complications, such as kidney disease.
- Bitter Melon: One supplement that has some solid research behind it, but I haven’t personally used myself or with clients, is bitter melon. Grown in Asia, India, Africa, and the Caribbean, this vegetable is generally used in curry dishes. All parts of the vegetable can be used (fruit for consumption and leaves for tea), and have been shown to possibly increase the release of insulin from the pancreas. It has also been found to oxidize glucose in red blood cells and adipose (fat) cells. This, in turn, helps those with type 2 diabetes to better manage their sugars by decreasing blood glucose levels and creating a better tolerance for glucose. It may also decrease HbA1c (average blood sugar) levels. For the most part, bitter melon is generally well-tolerated; however, gastrointestinal upset may occur. Though rare, reported side effects have included ulcers, rapid heartbeat, and kidney injury. There are a small number of reports of toxicity in both children and adults. Do not use bitter melon if you are pregnant. (66,67)
Blood Sugar-Friendly Foods
There is a wide variety of nourishing foods to choose from that will help keep your blood sugar levels in balance, but I recommend staying away from processed carbohydrates.
Natural carbohydrates, such as sweet potatoes and berries, can be eaten in moderation. For best results, you may want to limit your servings of carbohydrates to one or two a day if you’re still in the early stages of your Hashimoto’s journey and experiencing blood sugar swings. For some of my clients, even too much fruit can throw them off!
As you heal, your tolerance for carbohydrates will improve, but your focus should still be on low-glycemic index foods.
It’s a good idea to keep low carbohydrate snacks on hand to balance blood sugar and beat cravings. My favorite blood sugar-stabilizing sources of fats and proteins, which can be combined to make delicious snacks, are:
- Avocados
- Chia seeds
- Chicken
- Coconut milk
- Coconut
- Duck fat
- Eggs and egg white proteins (if not sensitive)
- Grass-fed beef
- Hydrolyzed beef protein
- Lamb
- Nuts (except peanuts)
- Olives and olive oil
- Pea protein
- Pork
- Salmon
- Sardines
- Seeds
- Stevia
- Tallow
- Turkey
- Whitefish
(Please note that some people may be intolerant to some of these foods and may need to complete an elimination diet or food sensitivity testing to find the right foods for their situation.)
Here is an example of how to rethink your breakfast and begin the day with a low-carbohydrate meal, that will start your day with balanced blood sugar levels and sustained energy:
Happy Breakfast = eggs + bacon + avocado + herbal tea with stevia
This is a healthier alternative to the typical Standard American Diet (S.A.D.) breakfast that may include a bagel with cream cheese, orange juice, and coffee with sugar!
In the same way, lunch and dinner can be made into blood sugar-balancing meals by swapping out high-carbohydrate foods for healthy fats and proteins, and small amounts of low GI carbohydrates. You can find more ideas on how to structure your meals in my Tasty Recipes article, or in my cookbook, Hashimoto’s Food Pharmacology: Nutrition Protocols and Healing Recipes to Take Charge of Your Thyroid Health.
For more information about low-carbohydrate foods that will help balance blood sugar levels and heal your thyroid, take a look at my Best Diet for Hashimoto’s article.
You can also download my free Hacking Diet eBook below!
The Takeaway
As you begin to move away from a carbohydrate-heavy diet and incorporate more low glycemic index foods, including plenty of healthy fats and proteins, into your meals, I encourage you to start journaling your symptoms. With balanced blood sugar, you may start to experience a reduction in thyroid antibodies and an improvement in energy levels almost immediately!
You can print the graphic of my blood sugar balancing rules below and hang it on your fridge to refer to at any time.
Increasing your intake of berberine, resistant starch, electrolytes, cinnamon, magnesium, probiotics, and the other nutrients listed earlier in this article, may also be beneficial.
Here’s another handy graphic that you can use to remind yourself of them:
Remember, blood sugar can be a significant issue for those with Hashimoto’s, but I’ve found that utilizing food as medicine is a simple and natural way to bring it into balance, reduce thyroid symptoms, and feel better.
I hope this information helps you on your journey!
P.S. You can download a free Thyroid Diet Guide, 10 thyroid-friendly recipes, and the Nutrient Depletions and Digestion chapter of my first book for free by signing up for my newsletter. You will also receive occasional updates about new research, resources, giveaways, and helpful information.
For future updates, make sure to follow us on Facebook and Instagram too!
References
- Penckofer S, Quinn L, Byrn M, Ferrans C, Miller M, Strange P. Does glycemic variability impact mood and quality of life? Diabetes Technol Ther. 2012;14(4):303-310. doi:10.1089/dia.2011.0191
- Aldossari KK, Shubair MM, Al-Zahrani J, et al. Association between Chronic Pain and Diabetes/Prediabetes: A Population-Based Cross-Sectional Survey in Saudi Arabia. Pain Res Manag. 2020;2020:8239474. Published 2020 Jun 24. doi:10.1155/2020/8239474
- Mergenthaler P, Lindauer U, Dienel GA, Meisel A. Sugar for the brain: the role of glucose in physiological and pathological brain function. Trends Neurosci. 2013;36(10):587-597. doi:10.1016/j.tins.2013.07.001
- Guilliams TG, Edwards L. Chronic Stress and The HPA Axis: Clinical Assessment and therapeutic Considerations. The Standard. Point Institute of Nutraceutical Research. 9(2): 2012.
- Physician Road Map. Interpretive Guide and Suggested Protocols for the Adrenal Recovery Kit Adrenal Stress Profile. Ortho Molecular Products. Third Edition. Accessed on 11/21/12 at www.orthomolecularproducts.com.
- Gierach M, Gierach J, Skowrońska A, et al. Hashimoto’s thyroiditis and carbohydrate metabolism disorders in patients hospitalised in the Department of Endocrinology and Diabetology of Ludwik Rydygier Collegium Medicum in Bydgoszcz between 2001 and 2010. Endokrynol Pol. 2012;63(1):14-17.
- Kadiyala R, Peter R, Okosieme OE. Thyroid dysfunction in patients with diabetes: clinical implications and screening strategies. Int J Clin Pract. 2010 Jul;64(8):1130-9. doi: 10.1111/j.1742-1241.2010.02376.x.
- Walter KN, Corwin EJ, Ulbrecht J, et al. Elevated thyroid stimulating hormone is associated with elevated cortisol in healthy young men and women. Thyroid Res. 2012;5(1):13. Published 2012 Oct 30. doi:10.1186/1756-6614-5-13
- Ranabir S, Reetu K. Stress and hormones. Indian J Endocrinol Metab. 2011;15(1):18-22. doi:10.4103/2230-8210.77573
- Thau L, Gandhi J, Sharma S. Physiology, Cortisol. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 6, 2021.
- Morey JN, Boggero IA, Scott AB, Segerstrom SC. Current Directions in Stress and Human Immune Function. Curr Opin Psychol. 2015;5:13-17. doi:10.1016/j.copsyc.2015.03.007
- Blood Sugar Major Player in Hashimoto’s Hypothyroidism. Functional Health News Website. http://functionalhealthnews.com/2014/08/blood-sugar-chronic-health/. Accessed February 5, 2019.
- Wilson, James. Adrenal Fatigue: The 21st Century Stress Syndrome. Smart Publications, 2011.
- Hyman, M. The Ultra Thyroid Solution: A 7-Step Plan To Reverse Hypothyroidism Permanently. Ultrawellness, LLC. 2008
- Altuntaş Y. Postprandial Reactive Hypoglycemia. Sisli Etfal Hastan Tip Bul. 2019;53(3):215-220. Published 2019 Aug 28. doi:10.14744/SEMB.2019.59455
- Lipska, KJ. Patient education: Hypoglycemia (low blood glucose) in people with diabetes (Beyond the Basics). UpToDate. Updated August 25, 2021. Accessed August 30, 2022.
- Hypos After Eating. Diabetes.co.uk. January 15, 2019. Updated June 10, 2022
- Biondi B, Kahaly GJ, Robertson RP. Thyroid Dysfunction and Diabetes Mellitus: Two Closely Associated Disorders. Endocr Rev. 2019;40(3):789-824. doi:10.1210/er.2018-00163
- Bugdaci MS, Zuhur SS, Sokmen M, Toksoy B, Bayraktar B, Altuntas Y. The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine [published correction appears in Helicobacter. 2011 Dec;16(6):482. Albayrak, Banu [corrected to Bayraktar, Banu]]. Helicobacter. 2011;16(2):124-130. doi:10.1111/j.1523-5378.2011.00830.x
- Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683-689. doi:10.2337/diacare.24.4.683.
- Witchel SF, Oberfield SE, Peña AS. Polycystic Ovary Syndrome: Pathophysiology, Presentation, and Treatment With Emphasis on Adolescent Girls. J Endocr Soc. 2019;3(8):1545-1573. Published 2019 Jun 14. doi:10.1210/js.2019-00078
- Williams T, Mortada R, Porter S. Diagnosis and Treatment of Polycystic Ovary Syndrome. Am Fam Physician. 2016;94(2):106-113.
- Krajmalnik-Brown R, Ilhan ZE, Kang DW, DiBaise JK. Effects of gut microbes on nutrient absorption and energy regulation. Nutr Clin Pract. 2012;27(2):201-214. doi:10.1177/0884533611436116
- Cohen, D. Gut Microbiome Controls Blood Glucose Levels Through the Liver. Weill Cornell Medicine. February 20, 2020. Accessed August 30, 2022.
- Mohammed L, Jha G, Malasevskaia I, Goud HK, Hassan A. The Interplay Between Sugar and Yeast Infections: Do Diabetics Have a Greater Predisposition to Develop Oral and Vulvovaginal Candidiasis?. Cureus. 2021;13(2):e13407. Published 2021 Feb 18. doi:10.7759/cureus.13407
- Nikolic DM. Effects of Candida on insulin secretion of human adult pancreatic islets and possible onset of diabetes. Br J Biomed Sci. 2014;71(2):73-78. doi:10.1080/09674845.2014.11669968
- Açbay O, Celik AF, Kadioğlu P, Göksel S, Gündoğdu S. Helicobacter pylori-induced gastritis may contribute to occurrence of postprandial symptomatic hypoglycemia. Dig Dis Sci. 1999;44(9):1837-1842. doi:10.1023/a:1018842606388
- Borghouts LB, Keizer HA. Exercise and insulin sensitivity: a review. Int J Sports Med. 2000;21(1):1-12. doi:10.1055/s-2000-8847Williams T, Mortada R, Porter S. Diagnosis and Treatment of Polycystic Ovary Syndrome. Am Fam Physician. 2016 Jul 15;94(2):106-13. PMID: 27419327.
- Exercise-induced hypoglycemia: What to know.Medical News Today. Updated January 12, 2022. Accessed August 30, 2022.
- Hill EE, Zack E, Battaglini C, Viru M, Viru A, Hackney AC. Exercise and circulating cortisol levels: the intensity threshold effect. J Endocrinol Invest. 2008;31(7):587-591. doi:10.1007/BF03345606
- Roussel R, Fezeu L, Bouby N, Balkau B, Lantieri O, Alhenc-Gelas F, et al. Low water intake and risk for new-onset hyperglycemia. Diabetes Care. 2011 Dec;34(12):2551-4. doi: 10.2337/dc11-0652. Epub 2011 Oct 12.
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354(9188):1435-1439. doi:10.1016/S0140-6736(99)01376-8
- Russell WR, Baka A, Björck I, et al. Impact of Diet Composition on Blood Glucose Regulation. Crit Rev Food Sci Nutr. 2016;56(4):541-590. doi:10.1080/10408398.2013.792772
- Martínez García RM, Jiménez Ortega AI, López Sobaler AM, Ortega RM. Estrategias nutricionales que mejoran la función cognitiva [Nutrition strategies that improve cognitive function]. Nutr Hosp. 2018;35(Spec No6):16-19. Published 2018 Sep 7. doi:10.20960/nh.2281
- Jones JL, Fernandez ML, McIntosh MS, et al. A Mediterranean-style low-glycemic-load diet improves variables of metabolic syndrome in women, and addition of a phytochemical-rich medical food enhances benefits on lipoprotein metabolism. J Clin Lipidol. 2011;5(3):188-196. doi:10.1016/j.jacl.2011.03.002
- Szypowska A, Regulska-Ilow B. Significance of low-carbohydrate diets and fasting in patients with cancer. Rocz Panstw Zakl Hig. 2019;70(4):325-336. doi:10.32394/rpzh.2019.0083
- Hruby A, Meigs JB, O’Donnell CJ, Jacques PF, McKeown NM. Higher magnesium intake reduces risk of impaired glucose and insulin metabolism and progression from prediabetes to diabetes in middle-aged americans. Diabetes Care. 2014;37(2):419-427. doi:10.2337/dc13-1397
- Guerrero-Romero F, Rodríguez-Morán M. Complementary therapies for diabetes: the case for chromium, magnesium, and antioxidants. Arch Med Res. 2005 May-Jun;36(3):250-7.
- Anderson RA, Polansky MM, Bryden NA, Bhathena SJ, Canary JJ. Effects of supplemental chromium on patients with symptoms of reactive hypoglycemia. Metabolism. 1987;36(4):351-355. doi:10.1016/0026-0495(87)90206-x
- Polegato BF, Pereira AG, Azevedo PS, et al. Role of Thiamin in Health and Disease. Nutr Clin Pract. 2019;34(4):558-564. doi:10.1002/ncp.10234
- Ringseis R, Keller J, Eder K. Role of carnitine in the regulation of glucose homeostasis and insulin sensitivity: evidence from in vivo and in vitro studies with carnitine supplementation and carnitine deficiency. Eur J Nutr. 2012 Feb;51(1):1-18. doi: 10.1007/s00394-011-0284-2.
- Magnusson M, Wang TJ, Clish C, et al. Dimethylglycine Deficiency and the Development of Diabetes. Diabetes. 2015;64(8):3010-3016. doi:10.2337/db14-1863
- Cools A, Maes D, Buyse J, Kalmar ID, Vandermeiren JA, Janssens GP. Effect of N,N-dimethylglycine supplementation in parturition feed for sows on metabolism, nutrient digestibility and reproductive performance. Animal. 2010;4(12):2004-2011. doi:10.1017/S1751731110001242
- Grizales AM, Patti ME, Lin AP, et al. Metabolic Effects of Betaine: A Randomized Clinical Trial of Betaine Supplementation in Prediabetes. J Clin Endocrinol Metab. 2018;103(8):3038-3049. doi:10.1210/jc.2018-00507
- Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717. doi:10.1016/j.metabol.2008.01.013
- Minozzi M, Nordio M, Pajalich R. The combined therapy myo-inositol plus D-Chiro-inositol, in a physiological ratio, reduces the cardiovascular risk by improving the lipid profile in PCOS patients. Eur Rev Med Pharmacol Sci. 2013 Feb;17(4):537-40.
- Unfer V, Facchinetti F, Ora B, Giordani B, Nestler J. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine Connections. 2017;6(8):647-658. doi:10.1530/EC-17-0243.
- Pizzo A, Laganà AS, Barbaro L. Comparison between effects of myo-inositol and D-chiro-inositol on ovarian function and metabolic factors in women with PCOS. Gynecol Endocrinol. 2014;30(3):205-208. doi:10.3109/09513590.2013.860120
- Matarrelli B, Vitacolonna E, D’Angelo M, et al. Effect of dietary myo-inositol supplementation in pregnancy on the incidence of maternal gestational diabetes mellitus and fetal outcomes: a randomized controlled trial. J Matern Fetal Neonatal Med. 2013;26(10):967-972. doi:10.3109/14767058.2013.766691.
- Mauras N, Xing D, Fox LA, Englert K, Darmaun D. Effects of glutamine on glycemic control during and after exercise in adolescents with type 1 diabetes: a pilot study. Diabetes Care. 2010;33(9):1951-3.
- Samocha-Bonet D, Chisholm DJ, Holst JJ, Greenfield JR5. L-glutamine and whole protein restore first-phase insulin response and increase glucagon-like peptide-1 in type 2 diabetes patients. Nutrients. 2015 Mar 24;7(4):2101-8. doi: 10.3390/nu7042101.
- Afkhami-Ardekani M, Shojaoddiny-Ardekani A. Effect of vitamin C on blood glucose, serum lipids & serum insulin in type 2 diabetes patients. Indian J Med Res. 2007;126(5):471-474.
- Yousefi Rad E, Djalali M, Koohdani F, et al. The Effects of Vitamin D Supplementation on Glucose Control and Insulin Resistance in Patients with Diabetes Type 2: A Randomized Clinical Trial Study. Iran J Public Health. 2014;43(12):1651-1656.
- Cruz KJC, de Oliveira ARS, Morais JBS, et al. Zinc and Insulin Resistance: Biochemical and Molecular Aspects. Biol Trace Elem Res. 2018;186(2):407-412. doi:10.1007/s12011-018-1308-z
- Nazem MR, Asadi M, Jabbari N, Allameh A. Effects of zinc supplementation on superoxide dismutase activity and gene expression, and metabolic parameters in overweight type 2 diabetes patients: A randomized, double-blind, controlled trial. Clin Biochem. 2019;69:15-20. doi:10.1016/j.clinbiochem.2019.05.008
- Zhang Y, Li X, Zou D, Liu W, Yang J, Zhu N, et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J Clin Endocrinol Metab. 2008 Jul;93(7):2559-65. doi: 10.1210/jc.2007-2404.
- Jia X, Zhai T, Qu C, et al. Metformin Reverses Hashimoto’s Thyroiditis by Regulating Key Immune Events. Front Cell Dev Biol. 2021;9:685522. Published 2021 May 28. doi:10.3389/fcell.2021.685522
- Robertson MD. Dietary-resistant starch and glucose metabolism. Curr Opin Clin Nutr Metab Care. 2012;15(4):362-367. doi:10.1097/MCO.0b013e3283536931
- Nugent, A. Health properties of resistant starch. Wiley Online Library. 2017. doi:10.1111/nbu.12244
- Kirkham S, Akilen R, Sharma S, Tsiami A. The potential of cinnamon to reduce blood glucose levels in patients with type 2 diabetes and insulin resistance. Diabetes Obes Metab. 2009 Dec;11(12):1100-13. doi: 10.1111/j.1463-1326.2009.01094.x.
- Daryabeygi-Khotbehsara R, Golzarand M, Ghaffari MP, Djafarian K. Nigella sativa improves glucose homeostasis and serum lipids in type 2 diabetes: A systematic review and meta-analysis. Complement Ther Med. 2017 Dec;35:6-13. doi: 10.1016/j.ctim.2017.08.016.
- Govindarajan S, Babu SN, Vijayalakshmi MA, Manohar P, Noor A. Aloe vera carbohydrates regulate glucose metabolism through improved glycogen synthesis and downregulation of hepatic gluconeogenesis in diabetic rats. J Ethnopharmacol. 2021;281:114556. doi:10.1016/j.jep.2021.114556
- Sáez-Lara MJ, Robles-Sanchez C, Ruiz-Ojeda FJ, Plaza-Diaz J, Gil A. Effects of Probiotics and Synbiotics on Obesity, Insulin Resistance Syndrome, Type 2 Diabetes and Non-Alcoholic Fatty Liver Disease: A Review of Human Clinical Trials. Int J Mol Sci. 2016;17(6):928. Published 2016 Jun 13. doi:10.3390/ijms17060928
- Aldini G, Altomare A, Baron G, et al. N-Acetylcysteine as an antioxidant and disulphide breaking agent: the reasons why. Free Radic Res. 2018;52(7):751-762. doi:10.1080/10715762.2018.1468564
- Tajmohammadi A, Razavi BM, Hosseinzadeh H. Silybum marianum (milk thistle) and its main constituent, silymarin, as a potential therapeutic plant in metabolic syndrome: A review. Phytother Res. 2018;32(10):1933-1949. doi:10.1002/ptr.6153
- Kim SK, Jung J, Jung JH, et al. Hypoglycemic efficacy and safety of Momordica charantia (bitter melon) in patients with type 2 diabetes mellitus. Complement Ther Med. 2020;52:102524. doi:10.1016/j.ctim.2020.102524
- Basch E, Gabardi S, Ulbricht C. Bitter melon (Momordica charantia): a review of efficacy and safety. Am J Health Syst Pharm. 2003;60(4):356-359. doi:10.1093/ajhp/60.4.356
- Roussel R, Fezeu L, Bouby N, Balkau B, Lantieri O, Alhenc-Gelas F, et al. Low water intake and risk for new-onset hyperglycemia. Diabetes Care. 2011 Dec;34(12):2551-4. doi: 10.2337/dc11-0652. Epub 2011 Oct 12.
- Ranasinghe P, Jayawardana R, Galappaththy P, Constantine GR, de Vas Gunawardana N, Katulanda P. Efficacy and safety of ‘true’ cinnamon (Cinnamomum zeylanicum) as a pharmaceutical agent in diabetes: a systematic review and meta-analysis. Diabet Med. 2012;29(12):1480-1492. doi:10.1111/j.1464-5491.2012.03718.x
- Nieman, LK. Patient education: Adrenal Insufficiency (Addison’s Disease)(Beyond the Basics). UpToDate. Updated May 26, 2021. Accessed August 30, 2022.
- Nieman, LK. Causes of Primary Adrenal Insufficiency (Addison’s Disease). UpToDate. Updated February 28, 2020. Accessed August 30, 2022.
- Nieman, LK. Pathogenesis of Adrenal Insufficiency. UpToDate. Updated August 29, 2022. Accessed August 30, 2022.
- Adaptogens. Therapeutic Research Center Natural Medicines Database. 2022. https://naturalmedicines-therapeuticresearch-com.mwu.idm.oclc.org/databases/food,-herbs-supplements/professional.aspx?productid=331
- Adrenal Extracts. Therapeutic Research Center Natural Medicines Database. 2022. https://naturalmedicines-therapeuticresearch-com.mwu.idm.oclc.org/databases/food,-herbs-supplements/professional.aspx?productid=941
- DHEA. Therapeutic Research Center Natural Medicines Database. 2022. https://naturalmedicines-therapeuticresearch-com.mwu.idm.oclc.org/databases/food,-herbs-supplements/professional.aspx?productid=331
- Wilder RL. Adrenal and gonadal steroid hormone deficiency in the pathogenesis of rheumatoid arthritis. J Rheumatol Suppl. 1996;44:10-12.
- Falorni A. Early Subclinical Addison’s disease. Endocrine Abstracts. 2009; 20:9.3.
- Penev P, Spiegel K, Marcinkowski T, Van Cauter E. Impact of carbohydrate-rich meals on plasma epinephrine levels: dysregulation with aging. J Clin Endocrinol Metab. 2005;90(11):6198-6206. doi:10.1210/jc.2005-0415.
- Molina PE. Chapter 4. Thyroid Gland. In: Molina PE, ed. Endocrine Physiology. 3rd Ed. New York: McGraw-Hill; 2010.
- Lizcano F, Rodríguez JS. Thyroid hormone therapy modulates hypothalamo-pituitary-adrenal axis. Endocr J. 2011;58(2):137-142. doi:10.1507/endocrj.k10e-369
Note: Originally published in May 2015, this article has been revised and updated for accuracy and thoroughness.


